Resident Research
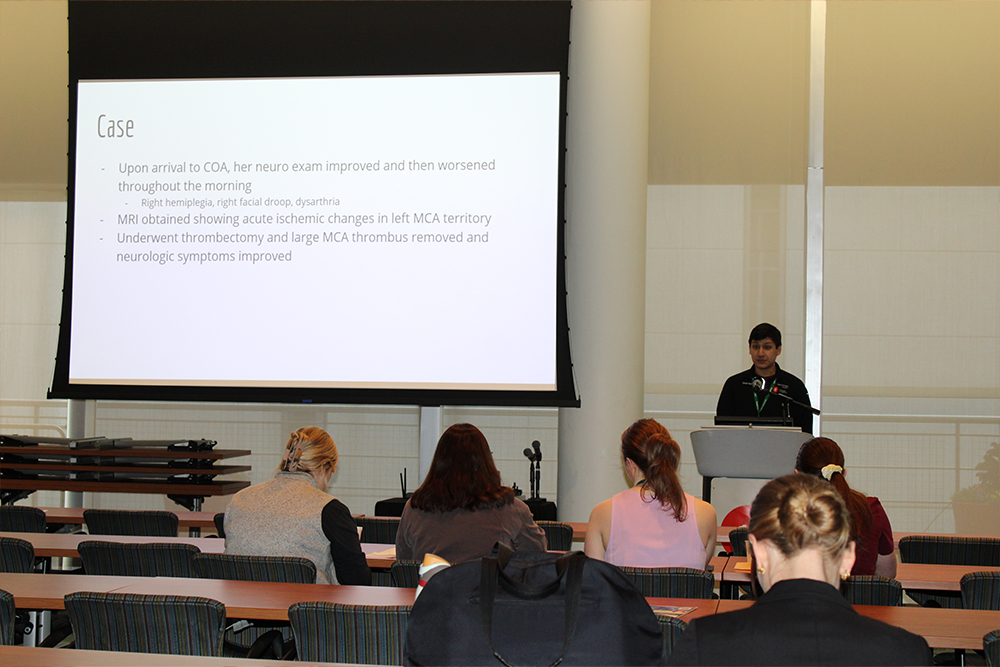
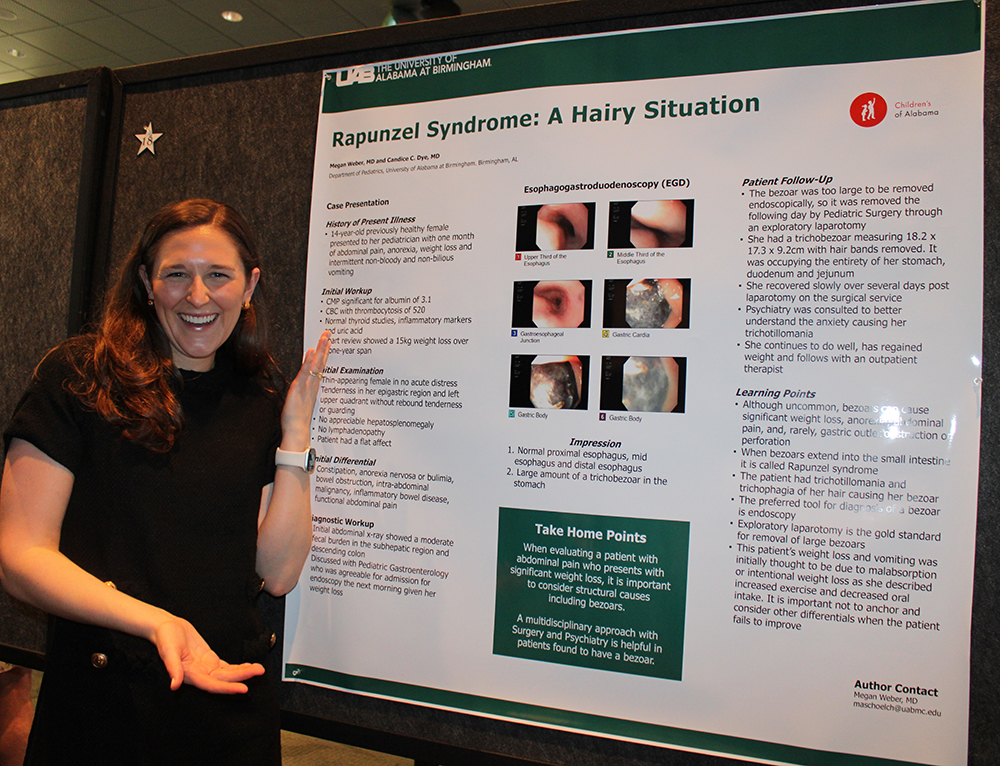
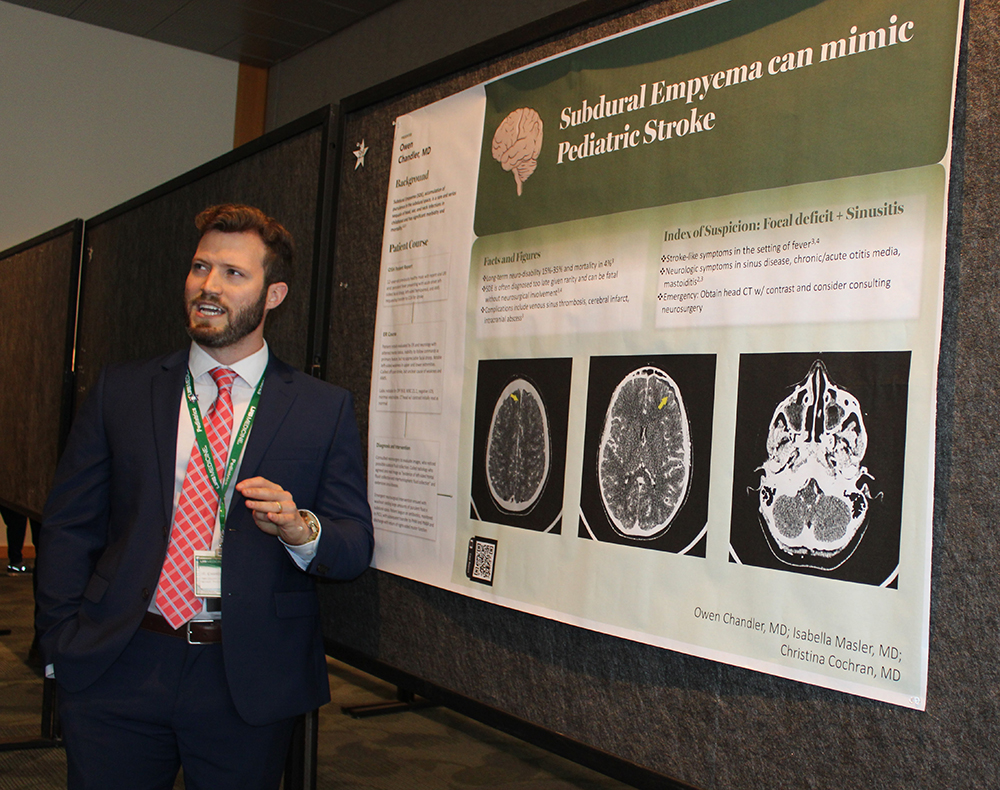
UAB and Children's of Alabama are leading research institutions in the country, placing UAB Pediatrics in the top 20 for NIH funding among pediatric departments. There are various opportunities for research available including bench, clinical, quality improvement, and simulation. We encourage resident participation in local and national meetings to present original research, attend poster sessions, or share interesting case presentations. The department offers reimbursement for conference and travel expenses. Below is a sampling of research and publications from residents over the last few years:
-
Notable Publications
Journal of Pediatric Surgery Case Reports. 2023 May;92:102602. Invasive pulmonary aspergillosis presenting with tracheopleural fistula in a pediatric patient with a history of rhabdomyosarcoma. Khatun M, Julson J, Taylor DW, et al.
The American Journal of the Medical Sciences, 365. (2023). A paralysis poser: A growing Covid Concern. Obremskey, N., Carpenter, A., & Wu, C.
American Journal of the Medical Sciences. 365 Supplement 1: S26, 2023. It's not the shunt: an atypical cause of fever in an infanct with hydrocephalus. Strange, K., Cooley, A.; Monroe, K; Shaughnessy, E.; Wu, C.L. (2023).
The American Journal of the Medical Sciences, 365. (2023). Altered mental status in the setting of pansinusitis and bilateral subdural empyemas. Thetford, K., Riegle, A., & May, B.
Founders' Fund
The Founders' Fund was established by the UAB Department of Pediatrics to honor the exceptional lifetime achievements of our department’s founders: Drs. John W. "Bill" Benton, Ralph E. Tiller, and Paul A. Palmisano. Educational grants of $1,000 from this fund support new, innovative educational research or programs related to the curriculum or quality and outcomes research of the residency program. Pediatric residents are eligible and frequently awarded Founders’ Fund grants. To date, 104 grants have been awarded!
-
2025-2026 Founders' Fund Projects
Increasing Use of Expedited Partner Therapy (EPT) for Sexually Transmitted Infection (STI) Treatment Among Adolescents
Lauren Brewer, MD (PI)
Daniel Cooper, MD (PI)
Kara Huls, MD (PI)
Heather Relyea Ashley, MD (PI)
Jamie McKinney, MD
Claudette Poole, MD
Deidre Schmidt PharmDWell Child Check that is Anything But Well: Use of Simulated Standardized Patients to Practice Empathetic Care of Sucicidal Teenager
Candice Dye, MD (PI)
A Deeper Dive into Caring for Patients from Vulnerable Populations
Jessica Corners, MD PGY3 (PI)
Amelia Hartje, MD PGY2
Kara Huls, MD
Nick Rockwell, MD
Lauren Robinson, MD
Chrystal Rutledge, MDImproving Car Seat Screening and Safety in Primary Care Clinic (PCC)
Lauren Dunavant, MD PGY 3 (PI)
Jemma Thompson, MD PGY 2 (PI)
Danielle Windom, MD PGY 2 (PI)
Callie Grey, MDImproving communication with LEP Families in the Pediatric ICU through simulation
Aya Al-Noubani, MD PGY5 Critical Care Fellow (PI)
Jessica Corners, MD PGY3
Lece Webb, MD
Jordan Newman, MDImproving Firearm Safety Counseling in PCC
Kathleen Vincent (Faculty PI)
Suzannah Patterson, MD PGY2
Reba Bosch, MD PGY2
Datlon Hall, MD PGY2
Michael Padgett, MD PGY2PREP for Fellowship
Anna Seidenburg, MD Chief Resident (PI)
David Taylor, MD PGY4 HO Fellow (PI)
Kelsey Thetford, MD PGY5 PHM Fellow (PI)
Jordan Newman, MD (Faculty PI)
Michele Nichols, MD (Facutly PI)Resident and Patient Education of Contraceptive Options in PCC
Katie Fogle, MD Chief Resident
Caroline Densmore, MD FacultyBaby Shower for Young Mothers Program
Sarah Hicks, MD PGY2 (PI)
Maddie Southall, MD PGY2 (PI)
Terri Coco, MD (Faculty PI)
Kathy Monroe, MD (Faculty PI)Communicating Difficult News: Comparing Skills Retention in Pediatric Residents
Allison Williams, MD PICU Fellow PGY5 (PI)
Anna Seidenburg, MD Chief Resident (PI)
Jordan Newman, MD
Emily Dodenhoff, MD
Emily Johnston, MD, MSPGY-1 101
David Taylor, MD PGY4 HO Fellow (PI)
Anna Seidenburg, MD Chief Resident (PI)
Jameson Ragsdale, MD Chief Resident (PI)
William Sasser, MD Faculty (PI)
Quality Improvement
To fulfill the ACGME quality improvement requirement, all residents participate in quality improvement projects during three years of residency. With a mentor’s guidance, residents lead and drive these projects through the Plan-Do-Study-Act cycle to obtain hands-on quality improvement experience. The program selects one project each year to receive the Quality Improvement Project Award. This award honors projects that exhibit exceptional quality improvement methods and improve the care of children in Alabama. Recent projects awarded by the program include the following:
-
Quality Improvement Award Winners
Increasing the Proportion of Postpartum Mothers with Opiate Use Disorder Receiving Naloxone by Discharge (2024)
Dr. Hannah Stone
Timely Identification of Technology Dependent BPD (2023)
Dr. Charli Cohen
High Risk Febrile Neonates (2022)
Drs. James Dunville, Jakob Evans
Inpatient Interventions for Improved Infant Safe Sleep (2021)
Drs. Meghan Harrison, Adria Luk, Isabella Masler, Kathryn Cyru
Pediatric Research Academic Program (Pediatric RAP)

This scholarly group meets monthly to discuss basic research topics, encourage research during residency, practice oral presentations, and network with each other and faculty. All residents are welcome!
Research Pathways
The UAB Pediatric Residency Program also accepts applicants into the two Research Pathways approved by the American Board of Pediatrics.
-
Accelerated Research Pathway (ARP)
-
This pathway is open to candidates who are committed to an academic career with a strong research emphasis. Residents would complete 2 years of General Pediatrics, then complete 4 years of subspecialty training.
-
Candidates MUST be identified no later than 9 months into their PGY I year, but preferably prior to their beginning their PGY I year.
-
This could occur at two different institutions.
-
For questions regarding the curriculum and further requirements, please refer to the ABP website or request further information from our UAB Pediatric Residency Program.
-
-
Integrated Research Pathway (IRP)
-
This pathway is designed to attract young physician scientists who want to sustain their research skills and productivity during Pediatric Residency.
-
This pathway is open to applicants with MD/PhD degrees or equivalent evidence of research experience and/ or commitment.
-
Candidates MUST be identified no later than 9 months into their PGY I year, but preferably prior to their beginning their PGY I year.
-
This pathway must occur at once institution.
-
The pathway duration would be 3 years with two years of general pediatrics (clinical) and up to one year of research.
-
For questions regarding the curriculum and further requirements, please refer to the ABP website or request further information from our UAB Pediatric Residency Program.
-
Additional Research Opportunity
The UAB Pediatric Residency Program also offers a “Research Gap Year,” which ideally would occur from July to the following June (12 months). If a resident has identified a mentor with whom he/she would like to complete a research project using protected time, the Department of Pediatrics will review the proposal and approve projects that meet requirements necessary for financial support and protected time. The resident would resume his or her pediatric residency responsibilities at the completion of the twelve months or project (or whichever comes first).
Stimulating Acess to Research in Residency (StARR)
The NIH NIAID R38-funded UAB StARR Program provides resident investigators with the opportunity to conduct mentored research related to infection, immunology and/or allergy and to participate in career development activities (in areas such as research methodology, scientific writing and team science) over a 12-month period during residency. The program aims to prepare resident investigators for a successful transition towards a career as an independent physician scientist that includes research that supports the NIH NIAID mission.
Click here for more information and application.