Division of Pediatric Critical Care
-
Beginnings of the Division
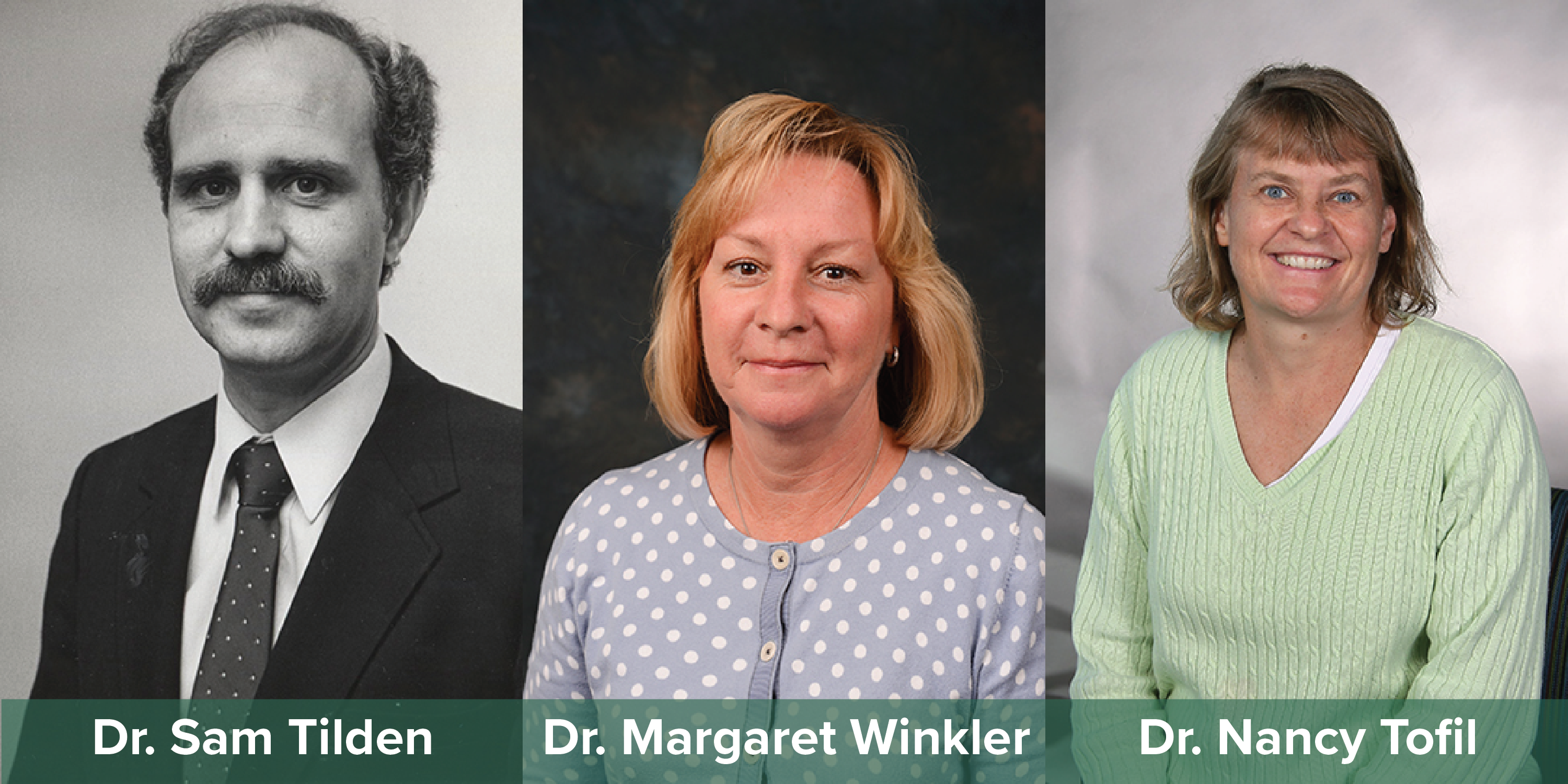
Pediatric Critical Care as a formal specialty at Children’s of Alabama and within the UAB Department of Pediatrics, began with the recruitment of Dr. Samuel Tilden as the first division director of Pediatric Critical Care in 1987. Dr. Tilden, a Louisiana native, graduated from Tulane University School of Medicine in 1977. He completed his pediatric residency at the Louisiana State University School of Medicine followed by a fellowship in pediatric pulmonology. He was recruited to the Department of Pediatrics from St. Joseph’s Hospital in Phoenix, Arizona, where he was director of the Pediatric Intensive Care Unit (PICU). The initial Pediatric Intensive Care Unit at Children’s of Alabama, developed and staffed under his direction, was an eight bed unit. It was expanded in the early 1990’s into a dedicated space consisting of 16 beds (12 ward type beds and four isolation rooms). Dr. Tilden recruited additional faculty with the hiring of Dr. Scott Curtis, who had completed training at the University of Pittsburgh in pediatric pulmonary and critical care, as well as Dr. James Royall, who had completed his pulmonary fellowship at UAB and elected to remain here.
With the beginnings of a critical mass of personnel established, Dr. Tilden began expanding the role of the division within the department. Fellowship training was established and the first fellows in pediatric critical care began their postgraduate training in 1990. In this early group of trainees was Dr. Steven Baldwin, who remains a member of the Department of Pediatric within the Division of Pediatric Emergency Medicine. The importance of fellowship training within the division has remained a point of emphasis since its early inception. The fellowship program to date has trained over 40 individuals who have gone on to establish successful private practice and academic careers at multiple institutions across the United States, Canada, Chile and Saudi Arabia. The quality of the division’s trainees is demonstrated by more than a quarter of them being recipients of the prestigious Dixon Fellowship grant, established in 1988 to support outstanding fellows for a career in academic medicine.
Additional faculty were recruited including Dr. Imad Haddad in 1993, Dr. Mark Buckmaster in 1995, who was trained in both pediatric anesthesia and critical care at the University of Minnesota, and Dr. Neil Kooy, who completed his fellowship at UAB in 1994 and returned in 1997. With these additional faculty members, Dr. Tilden continued to expand the scope of the division with coverage to include involvement with pediatric cardiac intensive care at University Hospital. This early consultative involvement provided the groundwork which later led to the establishment of a Pediatric Cardiac Intensive Care Unit at University Hospital and significant advancement of critical care services for infants and children with a wide variety of congenital heart disease.
In recognition that the provision of critical care services was important regardless of the location of the patient and the sooner such resources could be mobilized for the patient, pediatric critical care transport services were created to provide high quality, rapid medical care to critically ill pediatric patients regardless of where in the state or neighboring states the patient originated. Initially a ground and fixed wing based service, rotor craft were later added in partnership with University Hospital and later as part of a dedicated Children’s of Alabama’s fleet.
-
New Leadership
In 1999, Dr. Tilden stepped down as division director of Pediatric Critical Care and Dr. Margaret Winkler, a former fellow from 1994-1997, assumed the position. Dr. Winkler, who returned to the department after a three-year tenure at the University of Kentucky, was directly responsible for one of the fastest periods of expansion in the history of the division. With aggressive recruitment from within the fellow ranks, as well as outside the department, she expanded faculty numbers by almost threefold during her period as division director and director of the Pediatric Intensive Care Unit. She also oversaw the expansion of the Pediatric Intensive Care Unit from its long standing 16 beds to a new 24 bed unit to meet ongoing clinical demands. She became the first recipient of the Ann Dial McMillan Endowed Chair in Pediatric Critical Care.
Dr. Winkler’s faculty recruits were highly successful in implementing a major expansion of the scope of the division’s services in a wide variety of clinical arenas:
Nancy Tofil, a former fellow, led the development of the Pediatric Simulation Center for simulation training and education and became associate director of the Pediatric Residency Program. The Simulation Center has subsequently been recognized internally, as well as nationally, for the outstanding quality of its educational experience.
Jeffrey Alten, recruited after completing his critical care fellowship at Texas Children’s in Houston in 2005, led the expansion and development of pediatric cardiac intensive care at University Hospital and later within the new Benjamin Russell Hospital for Children campus, where a separate 20 bed Cardiac Critical Care unit and 10 bed monitored unit provides comprehensive care to children of all ages with simple and complex congenital heart disease. The unit is now a component of the Division of Pediatric Cardiology and oversees care to approximately 600 open heart cases per year. It is under the direction of Santiago Borasino, also recruited to the department by Dr. Winkler from Children’s Hospital of Philadelphia, after finishing a pediatric residency at UAB.
Tasked with the development of a procedural sedation service outside the operating room, the Simon Sedation service was created in 2003 under the medical direction of Mark Buckmaster. The service provides clinical services for approximately 1,200-1,600 cases per year to children requiring sedation for a wide variety of therapeutic and diagnostic services.
With the ongoing need and interest in pediatric critical care subspecialty training, Priya Prabhakaran was appointed director of the Pediatric Critical Care Fellowship Program. Under her guidance, the fellowship program has increased to six fellows. Interest in training at UAB has remained high, reflective of the quality of clinical material available and the dedication of faculty to the commitment of fellowship training remaining an educational experience that meets any goals incoming fellows may have.
The increasing supervisory insight mandated by more public and governmental regulatory agencies, led to Leslie Hayes, a former fellow who was recruited to the faculty, assuming the lead role in hospital quality improvement and patient safety initiatives as the first medical safety office for Children’s of Alabama. Dr. Hayes later became integral in the establishment of formal academic training programs in quality improvement and patient safety for UAB Health System and is currently the associate quality education officer for UAB Medicine.
Research remains an essential component of academic medicine and Michele Kong, recruited by Dr. Winkler after completion of her fellowship at UAB, has been pivotal in cementing research into the divisional foundation. Dr. Kong’s work in protease dysregulation in acute lung injury and the role of RSV induced respiratory failure in children has been recognized both internally and nationally and has led to multiple grant awards as a result. Dr. Kong, has also been responsible for establishment of KultureCity, a private foundation which provides financial, educational, and emotional support for families with children diagnosed with Autism Spectrum disorder.
William Sasser organizes the educational activities of the division as it relates to the School of Medicine and is highly involved with the organization of family centered services within the PICU.
Chrystal Rutledge has assumed the role of director of pediatric critical care transport, which in conjunction with her efforts in pediatric simulation has led to the fusion of these interests into programs providing outreach to community hospitals to improve early care for children presenting with critical illness. She along with Kristen Waddell, CRNP and Stacy Gaither, RN, has developed COACHES (Children’s of Alabama Community Healthcare Education Simulation Program) which uses simulated pediatric emergencies to train staff in emergency departments and inpatient areas in hospitals throughout the state.
-
Growth of the Department
This rapid expansion of the division culminated with the completion of the Benjamin Russell Hospital for Children in 2012 and the opening of a new state of the art Pediatric Critical Care Unit consisting of 24 expansive private rooms. These new rooms offer comfortable and private surroundings for the families of critically ill children. In 2017, Dr. Winkler stepped down as division director and was followed by Dr. Nancy Tofil. Dr. Tofil has continued to grow the role of the division within the department, as well as integrating the operation of critical care services more seamlessly into the overall operation of the hospital. She has continued to add to the roster of the division with ongoing recruitment of faculty, such as:
Robert Richter, a former fellow, leads the development of integrated ECMO services within the PICU. Prior to his fellowship he completed his pediatrics residency at Cincinnati Children’s Hospital in Ohio. In addition to his work with ECMO, he also engages in translational research evaluating the vascular endothelium in sepsis. In his first year, he obtained funding from the Kaul Pediatric Research Institute for his research and has subsequently received K08 funding and a NIH Loan Forgiveness Grant.
Madhura Hallman completed her pediatric residency at UAB and her subsequent pediatric critical care fellowship at LeBonheur Children’s Hospital at the University of Tennessee in Memphis. Dr. Hallman is leading a multidisciplinary effort to develop a decision support process regarding tracheostomy and long-term ventilation in children. She is the director of Family Engagement. In 2023, she along with partners from Hospital Medicine develop the Complex Care Service (Teal Team) which is an amazing team helping better care for the patient and families of some of the most medically complex children in Alabama.
Jeremy Loberger, a former fellow, is the Medical Director of the PICU. Prior to his fellowship he completed his internal medicine/pediatrics training at Greenville, South Carolina. He has helped lead along with the NICU and CVICU Medical Directors and hospital leadership a formalized surge plan taking advantage of all ICU beds in the hospital. He leads VentLib4Kids, a multicenter collaborative focused on early liberation from mechanical ventilation for children in the PICU. This has led to a decrease of almost an entire day for our patients, allowing them to leave the ICU sooner and making their care safer.
Vidit Bhargava completed his pediatric critical care fellowship at Stanford University in Palo Alto, California. He was a pediatric resident at the University of Texas at Galveston. He is the Director of our PICU Point of Care Ultrasound Program (POCUS) and is a national expert on this subject as it pertains to research and education. He is also the PICU Medical Director of the Liver Transplant Program.
Jordan Newman completed his fellowship at Emory University in Atlanta, Georgia. Prior to that he was a pediatric resident at the University of South Carolina in Charleston where he also was a chief resident. He is the Associate Director of the Pediatric Simulation Center and certified in TeamSTEPPS. He is also the Associate Fellowship Director and the Assistant PICU ECMO Director.
James Odum completed his fellowship at Cincinnati Children’s Hospital. Prior to that he was a pediatric resident at Children’s Mercy Hospital in Kansas City, Missouri where he was also a chief resident. He is engaged in translational research evaluating the interaction of sepsis and acute kidney injury. In his first year, he obtained funding from the Kaul Pediatric Research Institute for his research and has subsequently received a NIH Loan Forgiveness Grant. He serves as a Co-Director of the Pediatric and Infant Center for Acute Nephrology (PICAN) at Children’s of Alabama.
Lece Webb completed her fellowship at UAB and prior to that completed her internal medicine/pediatrics training at Greenville, South Carolina. She is very involved with diversity efforts. She is the director of the fellowship DEI council. She studies the role of health care disparities in pediatric critical care outcomes. In her first year, she obtained funding from the Kaul Pediatric Research Institute for her research.
Nick Rockwell completed both his fellowship and pediatric residency at UAB. Nick is the Associate Director of the Pediatric Simulation Center and very interested in expanding the role of simulation throughout the hospital. He is also the Co-Director of the 4th year medical student Prep for Residency Course which is required for all graduating medical students.
Emily Dodenhoff completed her PICU fellowship at UAB before doing an additional fellowship in Hospice and Palliative Medicine. Her primary academic appointment is with the Department of Internal Medicine, Division of Geriatric, Gerontology, and Palliative Medicine with a secondary appointment with Department of Pediatrics, Division of Critical Care. She splits her time evenly. She is also the Associate Program Director of the Hospice and Palliative Medicine Fellowship Program.
Luke Burton completed his fellowship at UAB. Prior to that he completed his internal medicine/pediatrics training at Greenville, South Carolina. He is the Medical Director of Pediatric Critical Care Transport. He is also the Associate Director of the PICU POCUS Program. His scholarly works involves investigating the role of bedside ultrasound to predict airway swelling surrounding extubation.
With the planned opening of the 12th floor 50-bed PICU in the spring of 2026, the Division of Pediatric Critical Care will need to continue to evolve, and ongoing recruitment is underway to meet the increasing needs for children with critical care medical illnesses.
-
Division Leadership
Division Directors
Sam Tilden- 1987-1999
Margaret Winkler- 1999-2017
Nancy Tofil- 2017 to present
Division of Pediatric Emergency Medicine
-
Beginnings of Pediatric Emergency Medicine in Alabama
Holy Innocents Hospital for Children was founded in 1911 located in the All Saints Parish House. Its name was changed to Children’s Hospital of Birmingham in 1914 and moved to a new building on 30th Street and 7thAvenue South in 1924. Outpatient services were first provided in 1925 but according to pediatrician Dr. Vince Carnaggio, “On 30th Street there really wasn’t an emergency department, you might meet a patient down there and then ask a nurse down from upstairs to help you out. You would see someone who just dropped in. The 30th Street facility would be sort of a source of referrals, but you just saw patients wherever they happened to show up.”
In 1959 the emergency department (ED) was in the “Hole” in the Hillman building, UAB’s first hospital. The Hillman Hospital was where the primarily African American children’s ward was located, though African American children were also provided care at Children’s Hospital. Children’s Hospital and UAB were separate entities until establishing a collaboration agreement when a new facility was opened in 1961, after which the majority of pediatric care was provided at Children’s Hospital, including emergency medicine.
The new facility was located on 6th Avenue South, between 16th and 17th streets. Between 1961 and 1982, the emergency department entrance was on 17th Street.A local pediatrician, Dr. Don Palmer, who started the Greenvale practice, was active in prevention efforts and began taking poison center calls (writing them on index cards) in 1958. The poison center started providing 24/7 access in 1978.
Paul Palmisano, M.D., MPH, arrived at UAB in 1966. Being both a pediatrician and pharmacologist, his focus was on poisoning prevention, as well as injury prevention and child safety in general. He recognized patterns that would cause injury to children and would develop strategies to avoid those injuries. He was known as a superb educator and patient advocate. He became the director of Student Affairs and assistant dean of the Heersink School of Medicine in 1973. His mentorship and passion for injury prevention continues today, the baton passing to Drs. Carden Johnston, Bill King, Michele Nichols and Kathy Monroe.
-
1970s
In 1970, Dr. Warren Derrick, after finishing an infectious disease fellowship with Dr. Hugh Dillon, took over the clinics and stayed on until 1976. He established an acute care “dispo” clinic, which provided episodic unscheduled primary care for minor illnesses. Residents would see patients in the acute care clinic until midnight when it closed and patients would then go to the ED. The acute care clinic consisted of four cubbyholes with curtains and no privacy, in addition to four holding cubicles, which were seldom used due to a lack of staffing. Residents performed all venipunctures and did their own gram stains.
Dr. Carden Johnston was originally hired as a hospitalist in 1974, but took over management of the clinic in 1977. The combined volume in the dispo clinic and ED that year was 20,000, with the large majority being seen in the dispo clinic.
In 1971, Geni Smith, RN, finished nursing school and started working at Children’s Hospital. After three weeks of floor nursing, she was taken to ED by the Director of Nursing, Ms. Petri, who informed Geni she would be running the unit on the 3-11 evening shift. The ED consisted of four rooms. When a patient arrived, following a brief observation, she would have to track down a physician appropriate to the complaint. Because there were no beepers, she would have to call to let a doctor know what was happening so the physician could make a decision about whether to come to see the patient. If a patient presented with an injury, Geni would see the child, take the appropriate x-ray and then call the orthopedic doctor, who would expect an interpretation of the radiograph. Then the orthopedist would come see the patient. Dr. Johnston’s son Robert was injured in a fall and was taken to the ED where Geni saw him, got an x-ray, diagnosed his fractured clavicle, put a figure-8 splint on him and sent him home with no physician involvement. Geni later became the trauma team coordinator and retired in 2017.
-
1980s
From 1978-1983, Dr. Carden Johnston was active lobbying the state to implement laws protecting children, requiring the use of car seats as one example. Dr. Johnston was the American Academy of Pediatrics (AAP) Alabama Chapter chairman from 1980 to 1983, and has represented Alabama on a multitude of national committees of the AAP and became the first Alabama Chapter member to become a national advocate for children as AAP President in 2003. In the early 1990s, he created and starred in an award winning weekly safety news segment educating the public about injury prevention on NBC 13 called KidCheck, which was nationally syndicated and ran for about 10 years. Dr. Johnston retired from clinical work in 2005, but as a professor emeritus continues to be active educating residents and students on child advocacy.
The ED changed location and size as part of a hospital expansion in 1982, moving the entrance from 17th Street over to 6th Avenue South. It went from four beds to eight emergency (medical and surgical) beds with an additional five beds for six-hour holding, and eight beds were referred to as the Acute Medical Clinic (ASM), which essentially moved the dispo clinic to be contiguous to the ED, and was staffed by residents who could consult general pediatrics faculty, Drs. Kathe Nelson and Coralie Hains. Showers for decontamination and negative pressure rooms were added at that time as well. According to Dr. Johnston, there was no sign indicating the ED entrance. Pediatric residents were seeing medical complaints, while the surgical and orthopedic residents were treating injuries. There were no attendings in the emergency department. Residents worked 36 hours taking breaks as they needed. Nurses were not allowed to start IVs, as decreed by Department Chair, Dr. Bill Benton, leaving that task to the residents. Neurosurgical patients would go to University Hospital where neurosurgery was located as there were no pediatric neurosurgeons. Private doctors would come to see their own patients in the ED.
The critical care transport team was started in 1983 but was part of the UAB transport team. It was staffed by moonlighting pediatric residents and the vast majority of pediatric transports were for neonatal patients. The ED and AMC saw 40,000 patients that year. National interest in pediatric emergency medicine was beginning to increase, with section status in the AAP starting in 1981 and the first textbook of pediatric emergency medicine published in 1983 by Steve Ludwig and Gary Fleisher, both at Children’s Hospital of Philadelphia at the time. The interest expanded to the pre-hospital environment the following year when Dr. Cal Sia and Hawaiian Senator Inouye introduced legislation for EMS-C (emergency medical services for children). The initial funding of the program began in 1986 and included a total of $2 million per year for state grants. Alabama and UAB received one of the four grants awarded that year, shared by surgeon Dr. Max Ramenofsky in Mobile, Alabama.
1986 was a big year in the growth of pediatric emergency medicine at UAB. Dr. Johnston was given permission to set up an emergency medical service at Children’s, which included a pediatric emergency medicine fellowship. The trauma center was also started that year with no medical involvement from the ED faculty. This was still before there was an attending present in the emergency department for anything other than consults. The residents ran unit and did not feel the need attendings to be present. The residents had the autonomy and responsibility to manage patients, make decisions and learn. Dr. Jake Vacarella, who completed his pediatric residency at UAB in 1982, joined the faculty in March 1987. He and Dr. Johnston decided to cover the ED from noon until midnight, 365 days a year, with one of them physically present in or near the department for 12 hours every day for over a year. Thanks to Drs. Johnston and Vacarella, who paved the way for us today!
Dr. Sergio Stagno’s appointment as chair of the Department of Pediatrics and physician in chief of the Children’s Hospital became official in 1989. Dr. Rud Polhill left private practice to join the department in 1989 and was appointed by Dr. Stagno as the director of both emergency medicine and general pediatrics. Dr. Polhill was one of the first two pediatric interns at the new Children’s Hospital facility and was chief resident in 1970-1971. He was in private practice for 13 years before joining the faculty. He died at the early age of 60 in 2002 from heart disease. The division continues to mourn his passing and celebrate his life and love of learning. Once a year we sponsor a memorial grand rounds speaker and present the Rud Polhill Award to a pediatric intern and a graduating emergency medicine resident who have demonstrated intellectual curiosity and a love of learning.
-
1990s
The emergency medicine faculty in 1990 included Drs. Johnston, Polhill, Vacarella, Karin McCloskey, who joined the faculty after being the first pediatric emergency medicine fellow at UAB, and Dr. Michele Nichols, who had just completed her pediatric emergency medicine fellowship at Cincinnati Children’s. Dr. McCloskey’s academic interest was critical care transport and she worked with the nurses to set up the transport team. She also advocated, applied for and created a section of transport in the AAP. Health issues forced her departure in 1994 and she died unexpectedly in 2007.
On her arrival, Dr. Nichols quickly became a leader in the division assuming responsibility for fellowship training, resident education and toxicology becoming the poison center medical director. Her compassion, work ethic, passion for teaching and academic focus in toxicology and poison prevention were more than reminiscent of Dr. Paul Palmisano.
Dr. Stagno appointed Dr. Nichols, along with Dr. Ray Watts, the assistant residency directors in 1992 and they assumed the role of co-program directors in 1995. Dr. Watts later stepped down and Dr. Nichols continued (to the present day) as the program director of one of the best pediatric residencies in the country. She continued as our fellowship director from 1991 – 2003, then as the co-director with Dr. Ann Klasner from 2003-2008, after which Dr. Klasner took over the role. Dr. Nichols remains the co-medical director of the Regional Poison Control Center. Dr. Stagno appointed her the vice-chair of Education for the department in 2014.
The American Heart Association (AHA) published the Pediatric Advance Life Support (PALS) course in 1998 which our division has been teaching to residents, physicians and nurses ever since. Dr. Vacarella was one of the first PALS national faculty. Dr. Kathy Monroe assumed administrative responsibility for the course when Dr. Vacarella left. Dr. Monroe handed it off to Dr. Annalise Sorrentino, who joined the faculty in 2003 after completing her pediatric emergency medicine fellowship at UAB. Dr. Sorrentino quickly became established as a leader in pediatric education and continues to be in demand as a speaker regionally, nationally and internationally. She is also active regionally and nationally with the American College of Emergency Physicians. Dr. Sorrentino handed administrative responsibility for the PALS course to Dr. Terri Coco, who joined the faculty in 2005 after completing her pediatric emergency medicine fellowship at UAB. Dr. Coco is the Regional AHA director (no longer have national faculty) and the director of all courses offered at Children’s of Alabama (~16/year). She is also co-director of our fellowship.
Bill King RPh, MPH, DrPH, worked as a pharmacist at Children’s Hospital, taught pharmacology at Samford, joined the UAB faculty in 1991 and further developed the Regional Poison Control Center. He obtained his graduate degree in Epidemiology with a thesis on e-codes (external cause of injury), which enables injury data collection. He created the Southeast Child Safety Institute with the goal of reducing injuries to children and along with Dr. Polhill established and managed the Pediatric Health Information Line (PHIL) in 1996. PHIL uses nurses, who follow Barton Schmitt telephone protocols, to provide advice to parents after their pediatrician’s office has closed. Data showed that PHIL reduced unnecessary use of the ED and appropriately referred patients to the ED who otherwise would have stayed home. Needless to say PHIL was warmly received by area pediatricians, and is still used today. Dr. King, who retired in 2017, provided invaluable epidemiological and statistical support for most of the clinical research conducted in the division.
The first pediatric emergency medicine sub-board certification occurred in 1992. The Division of Pediatric Emergency Medicine was officially established in 1993, and Dr. Stagno appointed Dr. Jake Vacarella as division director effective June 1st. Faculty at that time included:
-
Jake Vacarella, Director
-
Tim Givens – Fellowship: Cincinnati Children’s
-
Bill Hardwick - Fellowship: UAB
-
Carden Johnston
-
Karin McCloskey - Fellowship: UAB
-
Michele Nichols – Fellowship: Cincinnati Children’s
-
Rud Polhill
-
Lisa Santer – Fellowship: Case Western Reserve
Dr. Vacarella decided to return to private practice pediatrics in Wisconsin in 1995 and Dr. Roger Berkow, a member of the Division of Hematology Oncology, was appointed acting division director and chair of the Pediatric Emergency Medicine Division Director Search Committee. At that point Drs. Lisa Santer and Karin McCloskey had left and Dr. Tim Givens moved to Louisville in early 1996 to become their fellowship director. Dr. Monroe joined the faculty after completing her pediatric emergency medicine fellowship at UAB in 1995, leaving a total of only five faculty remaining in the division. Dr. Monroe quickly took on leadership roles in PALS, research, injury /advocacy and the AAP. The ED continued to be resident run with injuries still being seen by surgical resident moonlighters. There was no faculty presence after midnight. More than 50,000 patients were being seen in the ED that year.
Dr. Pete Glaeser, who had practiced pediatric emergency medicine at the Children’s Hospital of Wisconsin/Medical College of Wisconsin for 12 years, was hired as the new division director arriving at UAB in the spring of 1996 (much to the relief of Roger Berkow!). The ED entrance was still on 6th Avenue and there were 20 rooms, including a five bed holding area and a two-bay trauma room. Children’s Hospital signed a contract in October of 1996 with Health Services Foundation (HSF) to provide financial support to enable the hiring of additional pediatric emergency medicine faculty to provide 24/7/365 attending coverage in the ED. Surgical moonlighters were phased out and pediatric residents began learning and performing laceration repair and other injury related procedures. ED attendings and fellows and pediatric residents also assumed additional trauma team roles.
By 1999 PEM Faculty included: (year joined faculty)
-
Steve Baldwin (1996) – Fellowship: in PEM and Critical Care, UAB
-
Jud Barber (1999) – Fellowship: UAB
-
David Bernard (1997) – Fellowship: Johns Hopkins
-
Kim Copeland (1996) – Fellowship: UAB
-
Michelle Embling (1999) - Fellowship: UAB
-
Pete Glaeser- Division Director
-
Bill Hardwick- Fellowship: UAB Carden Johnston
-
Ann Klasner (1998) – Fellowship: Cardinal Glennon
-
Kathy Monroe (1995) – Fellowship: UAB
-
Michele Nichols - Fellowship: Cincinnati Children’s
-
Rud Polhill
The division took over management of the Vestavia After Hours clinic in 1999, which later moved to Children’s South after its completion. Another major event for the division and the department occurred in 1999 when a contract was negotiated with Children’s Hospital and the HSF to assume the costs of the division, including all costs associated with the fellowship. The only costs not included were academic efforts that had no relation to Children’s and the provision of patient care services. The hospital billed for and kept the clinical revenue generated by the division and reimbursed the department for the difference between revenue and costs. This funds flow arrangement continues to date and has morphed to include the hospital covering most academic, outreach, clinical and administrative activities of the faculty.
-
-
2000s
Dr. Don Arnold, who had practiced pediatrics and consulted in child abuse cases in Florida for years, started his pediatric emergency medicine fellowship at UAB in 1999. Dr. David Bernard was his faculty mentor and they recognized the need for the standardized care of children brought to the ED with a complaint of concern for sexual abuse/assault. Given the large number of providers assessing these children, all with varying levels of experience and expertise, and the time it takes to appropriately evaluate these patients in a busy ED, an effective standardized care pathway required a circle the wagons approach. For his fellow quality improvement project, Dr. Arnold implemented a SANE (Sexual Assault Nurse Examiner) program in the ED, which reduced the number of providers seeing these patients to those specially trained to do so. Dr. Bernard took over when Dr. Arnold completed his fellowship and left for a faculty position at Vanderbilt University. In addition to training the nurse examiners, all examinations are videotaped and Dr. Bernard reviews each one to confirm the findings. Most recently, Dr. Bernard has expanded the training and oversight/peer review to other locations in the state. In 2004, he was also named the medical director of the CHIPS Center (Children’s Hospital Intervention & Prevention Services) where he sees patients referred to the outpatient clinic. He obtained AAP Sub-Board Certification in Child Abuse in 2013. Dr. Melissa Peters joined the faculty in 2004 after her pediatric emergency medicine fellowship at the Children’s Hospital of the King’s Daughters in Norfolk, Virginia. She was also passionate about providing expert care for children who are suspected of being physically abused and splits her time between the ED and CHIPS, becoming the medical director for Physical Abuse Services in 2004. She provides inpatient consultation for suspected child abuse and became board certified in Child Abuse in 2013. Dr. Cohen created a new Division of Child Abuse in 2015 and recruited Dr. Mike Taylor from the Medical University of South Carolina to become the new director.
In 2003 a major renovation of ED was completed increasing its size by 30%. Over 53,000 patients were seen in the ED that year. The fellowship was expanded to three positions per year in 2003.
The ED volume took an unexpected dip in 2004 to 46,000 patients seen. This was fortunate in some ways because resident coverage of the ED decreased by 2/3rds that year, marking the end of anything that resembled a resident run ED. To partially compensate for the decrease in ED providers, we began using nurse practitioners (NPs) that year. Though controversial at the time, the NPs have proven themselves as capable and valuable independent care providers. We started with three NPs and now have 15 with 24/7 coverage.The division expanded its clinical coverage in 2006 to include a deep sedation service for radiology patients. Dr. Jud Barber is the division’s director of Sedation and also chairs the hospital’s sedation committee. We continue to provide this service at Children’s South five days a week. 2006 also saw the creation of the Pediatric Simulation Center established at Children’s Hospital. Dr. Marjorie Lee White joined the faculty in 2008 after completing a combined critical care and pediatric emergency medicine fellowship and co-directed the Simulation Center with Dr. Nancy Tofil. Subsequently Dr. White became the assistant dean and vice president for Clinical Simulation for the School of Medicine and the UAB Health System and also holds the title of director of the UAB Office of Inter-professional Simulation for Innovative Clinical Practice, Center for Inter-professional Education and Simulation.
Dr. Stagno appointed Dr. Pete Glaeser as the vice-chair for Clinical Services for the department in 2008. He continues as division director and appointed Dr. Monroe as the medical director of the ED. Dr. Monroe had been the division’s research director, which was transitioned to Dr. Chris Pruitt, who joined the faculty in 2010 after completing his pediatric emergency medicine fellowship at UAB. Drs Monroe and Nichols continue as the pied pipers of resident and medical student research and outreach advocacy.
-
2010s
The division was honored in 2010 with the creation of the C. Phillip McWane Endowed Chair in Pediatric Emergency Medicine. Dr. Glaeser was named the first recipient of the chair.
The beautiful Benjamin Russell Hospital for Children opened in August of 2012. The new ED contains 53 rooms, including four major resuscitation areas in close proximity to a separate ambulance entrance, an elevator that goes directly to the heliport and radiology. This increase in capacity was predictably met with substantially increased ED volumes. The highest volume in prior years was 57,000 and we are now seeing 74,000 patients per year. Obviously this has required additional providers and faculty. The decision was made in 2017 to close the After Hours Clinic and use the pediatricians to staff the lower acuity area of the ED. Four specially designed rooms with their own nursing station and lockable entrances were created to care for the burgeoning number of patients presenting with behavioral and psychiatric complaints. Unfortunately, these complaints continue to expand far exceeding the four bed capacity and the lack of inpatient beds results in these patients being held in the ED, often times for days.
Current PEM Faculty
(year joined faculty)
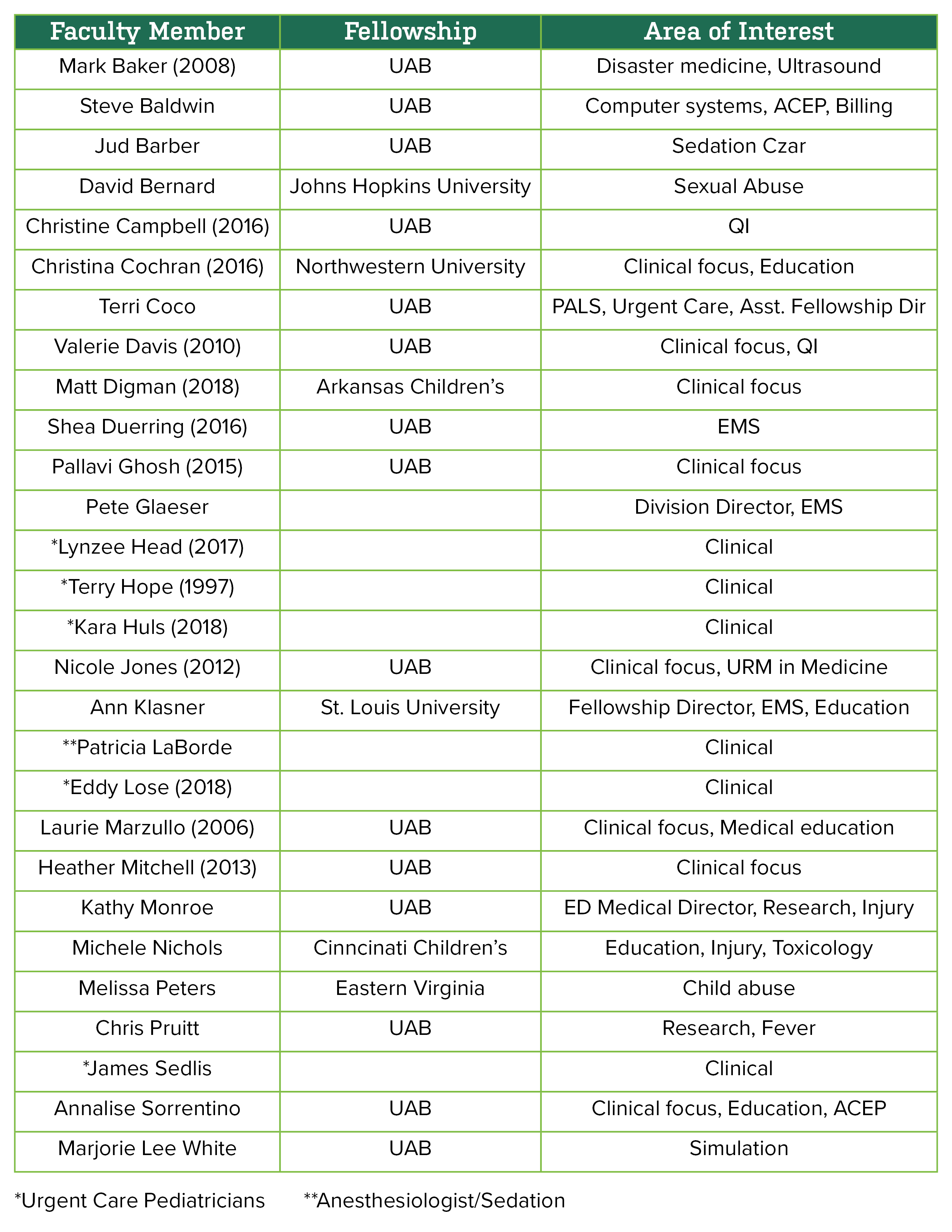
Additional division team members include: Jackie Freeman, Administrative Supervisor, Megan Beal, Office Associate II, Keandra Simmons, Office SVCS Specialist, Brittany Appelboom, Fellowship Program Coordinator, and Nipam Shah, Research Associate.
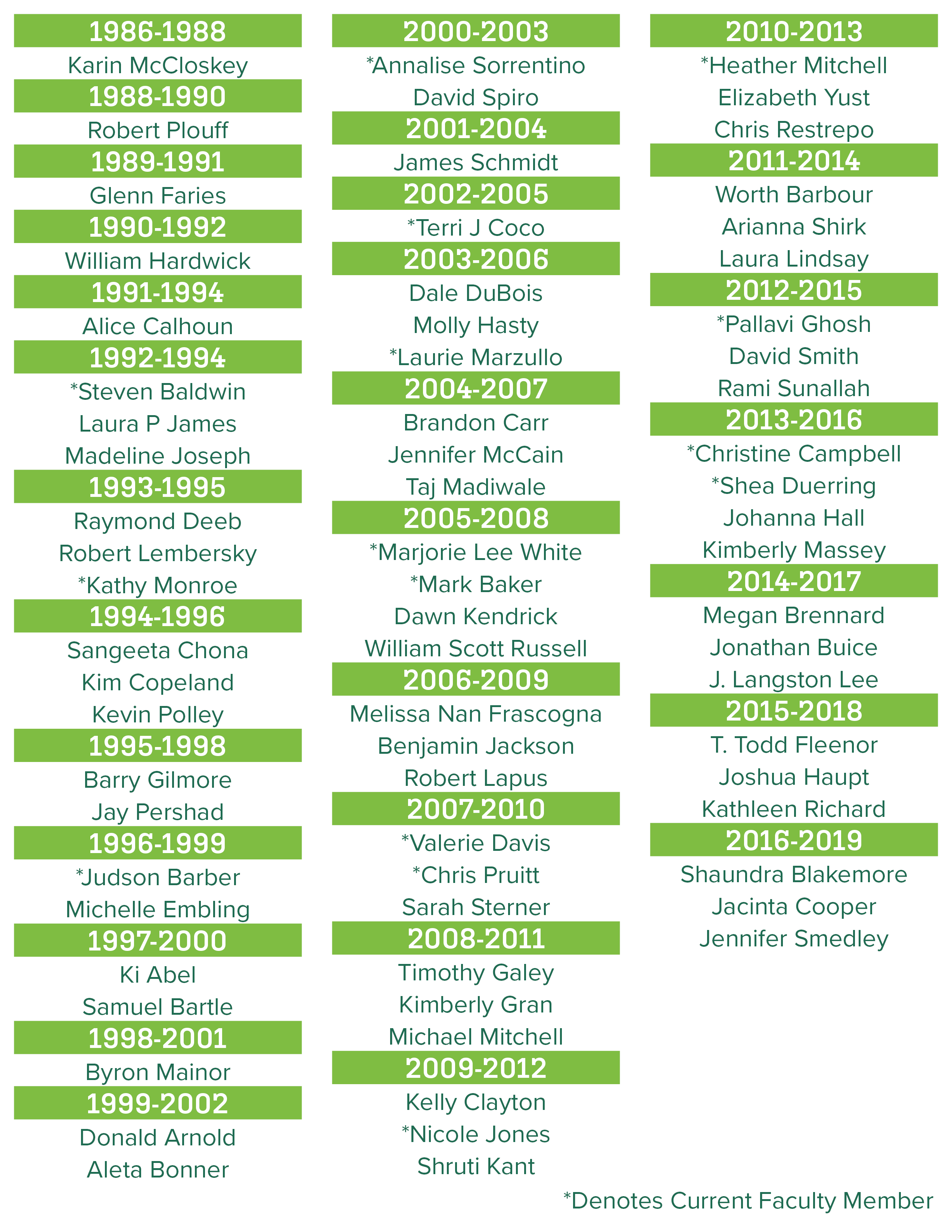
Fellows Who Have Trained With Us
Click here for a list with their current position
Division of Pediatric Endocrinology & Diabetes
-
History
The Division of Pediatric Endocrinology at UAB was formally established in 1964 with the arrival of Dr. Russell Cunningham, the first trained pediatric endocrinologist in Alabama. A native of Bayou La Batre, Dr. Cunningham returned to the state following his fellowship at Boston Children’s Hospital and laid the foundation for specialized care in pediatric endocrinology. For over two decades, he served as a one-person division, delivering expert care to children with diabetes and other endocrine disorders. He pioneered a model of comprehensive, family-centered endocrine care long before it became standard. In 1990, Drs. Katrina Parker and Joycelyn Atchison joined the division, bringing a collaborative dimension to endocrine care. Following his passing in 2006, the Russell Cunningham Memorial Research Scholarship was established to support medical students with an interest in academic pediatrics.
In mid-2000s, Dr. Kenneth McCormick was appointed as the division director of the Division of Pediatric Endocrinology. While in Wisconsin, he had been director of the core laboratory for a seven year, state-wide, NIH-funded, non-interventional, longitudinal study of Type 1 diabetes sequelae. Approximately seven months thereafter, with the addition of Dr. Gail Mick, the division had expanded to five members, some of which were part-time. Dr. Ambika Ashraf (2019–present) currently serves as the Division Director and the Ralph Frohsin Endowed Chair in Pediatric Endocrinology.
Today, the Division of Pediatric Endocrinology and Diabetes is recognized as a regional and national leader in comprehensive care, cutting-edge research, and trainee development. With 11 pediatric endocrinologists, 11 nurse practitioners, and over 15 diabetes educators, the division delivers care across a wide spectrum of endocrine disorders.
With robust clinical volume, growing research collaborations, and a thriving fellowship program, the Division continues to build on its legacy while innovating for the future. The support of the Ralph Frohsin Endowment and Bruno fellows have been instrumental in propelling initiatives that improve care, expand knowledge, and train the next generation of pediatric endocrinologists.
-
Clinical Care
We manage over 15000 outpatient visits annually, including 6,500 diabetes-specific visits, and more than 550 diabetes-related inpatient admissions. Our clinics are both high-volume and high specialty, including:
- Diabetes clinics
- High-risk Diabetes Clinic
- High A1C Clinic
- Type 2 Diabetes clinic
- Prediabetes Clinics
- Turner Syndrome Clinic
- Metabolic Bone Disease Clinic
- Lipid Disorders Clinic
- Newborn Screening Follow-Up Clinic
- Polycystic Ovary Syndrome (PCOS) Clinic
- Thyroid Nodule and Thyroid Cancer Program
- Cancer survivorship clinic
-
Education
In 2001, the most pressing mission was to develop a fellowship program given the relentless decline in pediatric residents wishing to pursue a career in endocrinology which, alarmingly, paralleled the aforementioned nationwide rise in the incidence of both type I and II diabetes. With the proliferation of endocrine disorders and concomitant decline in the number of young endocrinologists, these antithetical trends did not bode well for endocrine care in Alabama. Fortuitously, and timely, funding for the three-year fellowship was ensured by an endowment from the Bruno Diabetes Foundation. Parenthetically, years before 2001, the largess of the Joseph Bruno family supported not only the endocrine fellowship but also multiple diabetes-related academic/clinical activities. Accreditation of the fellowship program was announced in 2002.
Endocrine fellows are listed in chronological order:
Ambika Ashraf 2003-2006
Whitney Brown 2005-2008
Amy Burton 2007-2010
James Gardner 2008-2011
Alison Lunsford 2010-2013
Caroline Colvin 2011-2014
Linnea Larson-Williams 2012-2015
Alexandra Martin 2013-2015
Shelly Mercer 2015-2018
Heather Choat 2016-2019
Bhuvana Sunil 2017-2020
Jessica Schmitt 2017-2020
Jurhee Freese 2018-2021
Erin Greenup 2018-2021
As of 2018, the division was comprised of nine board-certified endocrinologists, one instructor, nine nurse practitioners, 12 clinic nurses, six hormone stimulation testing nurses, 14 diabetes educators, five diabetes pump nurses, two nutritionists, two social workers, and one shared child family therapists. Note: many of the staff are part-time.
Fellowship Pogram
Our ACGME-accredited fellowship program currently has the capacity to train six fellows across three years, with a curriculum emphasizing clinical acumen, multidisciplinary exposure, scholarly productivity, and professional growth. We consider ourselves to be a “fellow driven” program, not “fellow dependent”, and value clinical exposure and education for our trainees, but we do not make them do more if there are fewer fellows. We support fellows’ involvement in programs and activities that will help best prepare them for a successful career in pediatric endocrinology.
Our faculty serve in national leadership roles across the American Board of Pediatrics, the Pediatric Endocrine Society and the American Academy of Pediatrics.
-
Research
Since 2001, research conducted by pediatric endocrinology faculty encompassed cystic fibrosis-related bone health/growth, treatment and etiology of type 1 diabetes (T1DM), lipoprotein metabolism, Vitamin D deficiency, congenital hypothyroidism, endoplasmic reticulum luminal redox effect on cortisol production in isolated microsomes and β-cell apoptosis in cystic fibrosis (CF).
Publications have appeared in several high-impact journals, including: J Peds, JAMA Pediatrics, Arch Internal Med, Journal of Biological Chemistry, Biochemical Journal, Journal of Steroid Biochemistry, Pediatrics, Journal of Clinical Endocrinology and Metabolism, PLOS ONE, Obesity, Journal of Clinical Lipidology, Endocrinology, Journal of Endocrinology and Biochim Biophysics Acta to name a few.
Ongoing research studies and clinical projects include such topics as:
- The biological defect in the CF transmembrane conductance regulator (CFTR) protein impact on both growth and bone health
- GABA intervention in new-onset Type1 diabetes to preserve β-cell function. This pioneering double-blind, placebo- controlled, project is the first clinical trial of oral gamma aminobutyric acid (GABA) to preserve or restore endogenous insulin secretion, reduce prandial glucagon secretion, improve metabolic/glycemic control, and modulate favorably the autoimmune milieu. This is an investigator initiated study funded through JDRF.
- Increased incidence of Type1 diabetes in African American youth, a cross-section investigation
- Anti-N-acetylglucosamine antibodies from B lymphocytes, their prevalence and their role in the etiology of Type1 diabetes
- Immunology of Type1 diabetes the first year post diagnosis
- Redox regulation of endoplasmic calcium ATPase and uptake in isolated hepatic microsomes
- Modulation of macronutrient composition for management of lipid disorders and non-alcoholic fatty liver disease.
- Natural history of Type1 diabetes (NIH multicenter study)
- 11-Ketotestosterone concentrations in children with CAH and other adrenal disorders
- Cystic fibrosis diabetes and β-cell apoptosis by assaying unmethylated insulin DNA(in collaboration with Pennington Biomedical Center)
- ECHO (Extension for Community Healthcare Outcomes) video-conferencing program covering Pediatric Diabetes and Obesity - Spring 2018
- Diagnostic value of a second newborn screening test for congenital hypothyroidism
- Vitamin D deficiency in pediatrics and its role in glucose homeostasis and vascular health
- Dyslipidemia, obesity, and pre-diabete
- Participation in at least 10 pharmaceutical-sponsored investigative drug studies concerning Type2 diabetes, growth hormone deficiency, hypophosphatasia, FGF23 excess, Prader Willi syndrome
Research Highlights
Our division participates in NIH grants, including:
- The Youth-Onset Type 2 Diabetes Consortium – Discovery study(U01DK134966, Ashraf/Gower)
- Dietary intervention trials in NAFLD (R01DK128457, Ashraf/Goss)
Other notable areas of research include:
- Epigenetics and social determinants of type 2 diabetes (Dr. Christy Foster)
- Gut microbiome studies in pediatric metabolic disease (Dr. Ambika Ashraf)
- Expanded access therapy for rare conditions such as MCT8 deficiency (Dr. Leen Matalka)
- Multicenter trials in CAH and thyroid disorders (Dr. Gail Mick)
- T1D Exchange (Dr. Mary Lauren Scott, Dr. Jessica Schmitt)
- QI projects (Dr. Jessica Schmitt, Dr. Christy Foster)
The division also leads in Quality Improvement initiatives through participation in the T1D Exchange, Type 2 Diabetes Education Collaboratives, and transition care innovations, ensuring equitable access to advanced diabetes technologies and empowering patients and caregivers alike.
Division of Pediatric Gastroenterology, Hepatology and Nutrition
The Division of Pediatric Gastroenterology, Hepatology and Nutrition is a relatively new entity. It has a history of being a small but robust program, with marked growth over the past decade. The following is the history of the division by decade.
-
1982-1989
The founding father of pediatric gastroenterology (GI) at UAB and Children’s of Alabama was Dr. Jose Mestre. He was recruited in 1982 to establish a brand new division. He joined as faculty following completion of his fellowship at the Medical College of Virginia in Richmond. He was instrumental in establishing not only the outpatient and inpatient GI services but also for bringing pediatric fiber-optic endoscopy to Birmingham. As an aside, Dr. Basil Hirschowitz invented and perfected fiber-optic endoscopy in adults at UAB in 1959. Dr. Mestre was the sole pediatric gastroenterologist in the state and the only faculty member in the division. In 1987, he left to start a private practice in town but continued resident teaching both in his practice and at UAB and Children’s of Alabama.
-
1990-1999
After Dr. Mestre’s departure, the division had no formal faculty until 1990, when Drs. Frank Franklin and Ray Figueroa joined the division. Dr. Franklin was appointed the new division director. His research and clinical interests were in nutrition and lipid metabolism. He was a recognized leader in the field and was very successful during this period with numerous publications and extramural funding. Dr. Figueroa’s interests were in nutrition and obesity and he had several grants to fund studies in obesity and metabolism.
During this decade, Dr. Franklin continued to lead as the division director. Additional faculty added to the division included Drs. James Wright and Pamela Brown. Dr. Brown’s research included a randomized controlled trial of glutamine in the treatment of pediatric patients with intestinal failure.
The division continued to provide medical student and resident training in both the inpatient and outpatient arenas. With the addition of new faculty, Dr. Franklin was able to establish the first pediatric gastroenterology fellowship at UAB. The first fellow was Dr. Paul Harris, who was involved in seminal research in collaboration with Dr. Phil Smith. Dr. Harris has gone on to be an international leader in pediatrics and pediatric GI after returning to Chile.
By the end of this decade, Drs. Roberto Guerrero and Cary Cavender joined the division. During this time, Dr. Brown left UAB and joined the faculty at the University of Michigan. Dr. Figueroa left academia for some time and took a position with Mead Johnson. Ultimately, Drs. Figueroa and Guerrero settled into private practices in Florida.
In 1997, the division experienced a tremendous loss with the death of Dr. Wright. Beyond being a national leader in pediatric GI, he was an exemplary physician, teacher, researcher, husband and father. To honor his life, the James Wright Lectureship was established. This program continues to support bringing leaders in pediatric GI, nutrition and hepatology to present at an annual Grand Rounds at Children’s of Alabama.
-
2000-2009
The new millennium brought growth and new challenges. Dr. Franklin’s passion for public health and nutrition resulted in being named the chair of Maternal and Child Health at the UAB School of Public Health. Dr. Tim Boyle was recruited from Tufts University to become the new division director in 2002. Dr. Boyle’s academic efforts were in gastrointestinal motility issues. In addition, Dr. Shehzad Saeed also joined the faculty from Tufts University. Dr. Saeed’s research and clinical focus was inflammatory bowel disease. Over the next few years, several previous pediatric GI fellows joined the faculty. The addition of Drs. Steven King, Jeanine Maclin and Jan Nogueira allowed the division to expand services including treating pediatric patients with liver disease. By partnering with the UAB Department of Surgery, the division was able to begin caring for pediatric liver transplant patients.
As mentioned, there were some noted challenges to the division during this period, Drs. King and Cavender left UAB to open yet another private practice in Birmingham. A few years later, Dr. Boyle accepted a faculty position at the Children’s Hospital of Philadelphia.
After the departure of Dr. Boyle, Dr. Saeed was selected to be the next division director. Under his leadership, the division continued to grow. In addition to the previous fellows joining the faculty, Dr. Kirk Thame was recruited from Jamaica. Dr. Thame completed fellowship at Washington University in St. Louis. His area of expertise was also in motility disorders of children.
At the end of decade, Dr. Saeed was recruited to Cincinnati Children’s Hospital as the medical director for their Inflammatory Bowel Disease (IBD) Program.
-
2010-2019
Dr. Reed Dimmitt was appointed to division director in 2010, after serving as the interim division director in 2009. That same year, Dr. Meredith Hitch was recruited to the faculty after completing a fellowship at Washington University. She was a member of the faculty for a few years until accepting a position in Baton Rouge, Louisiana. Dr. Thame left soon after for a faculty position at Vanderbilt University. Dr. Traci Jester completed her training at UAB and joined shortly thereafter. The addition of new faculty allowed the division to develop new sub-specialty programs. To this end, Dr. David Galloway was recruited to direct the Intestinal Rehabilitation Program. Drs. Jester and Maclin developed a dedicated Inflammatory Bowel Disease Program that is nationally recognized by the multi-center collaborative Improve Care Now.
In 2013, Dr. Mitch Cohen was recruited to be the new chairman of Pediatrics at UAB, as well as another pediatric GI faculty member. Under his leadership, UAB was able to bring Dr. Jose Mestre back to UAB. The addition of Dr. Mestre was the catalyst for the most rapid growth ever for the division. Over the past five years a number of additional programs were established and new faculty were specifically recruited to lead them. Dr. Rachel Kassel joined the faculty from Washington University to be the medical director of the Intensive Feeding Program. Dr. Nick CaJacob finished fellowship at UAB and directs the Eosinophilic GI Disease Program. Lastly, Drs. Mike Leonis and Gillian Noel joined Dr. Nogueira to form a robust Liver Disease Program.
Because of our rapid growth, the division was able to develop some novel approaches. We now have two pediatric psychologists, Drs. Margaux Barnes and Marissa Gowey. They are primarily research focused, studying weight management and IBD, respectively. We also have been successful in hiring general pediatricians that are embedded in the outpatient clinics. Dr. Erin Bhatia was the first general pediatrician and was in the division for two years while her husband was completing a surgical fellowship at UAB. We were fortunate to recruit Dr. Amanda Soong from private practice to serve the same role.
Our fellowship program has also grown and now has two positions each year. Our graduating fellows have almost exclusively accepted academic positions. Included in this group are:
Paul Harris, M.D. | Catholic University, Santiago, Chile
Brian Morris, M.D. | Ochsner Hospital
Jeanine Maclin, M.D. | UAB
Jan Nogueira, M.D. | UAB
Reed Dimmitt, M.D. | UAB
Traci Jester, M.D. | UAB
Nick CaJacob, M.D. | UAB
Erika Smith, M.D. | Ochsner Hospital
Naren Vadlamudi, M.D. | Virginia Commonwealth University
Nagraj Kasi, M.D. | Medical University of South Carolina
Osman Ahmad, M.D. | University of Florida
Saurahb Talathi, M.D. | University of Oklahoma
Division of Neonatology
-
Beginnings of the Division
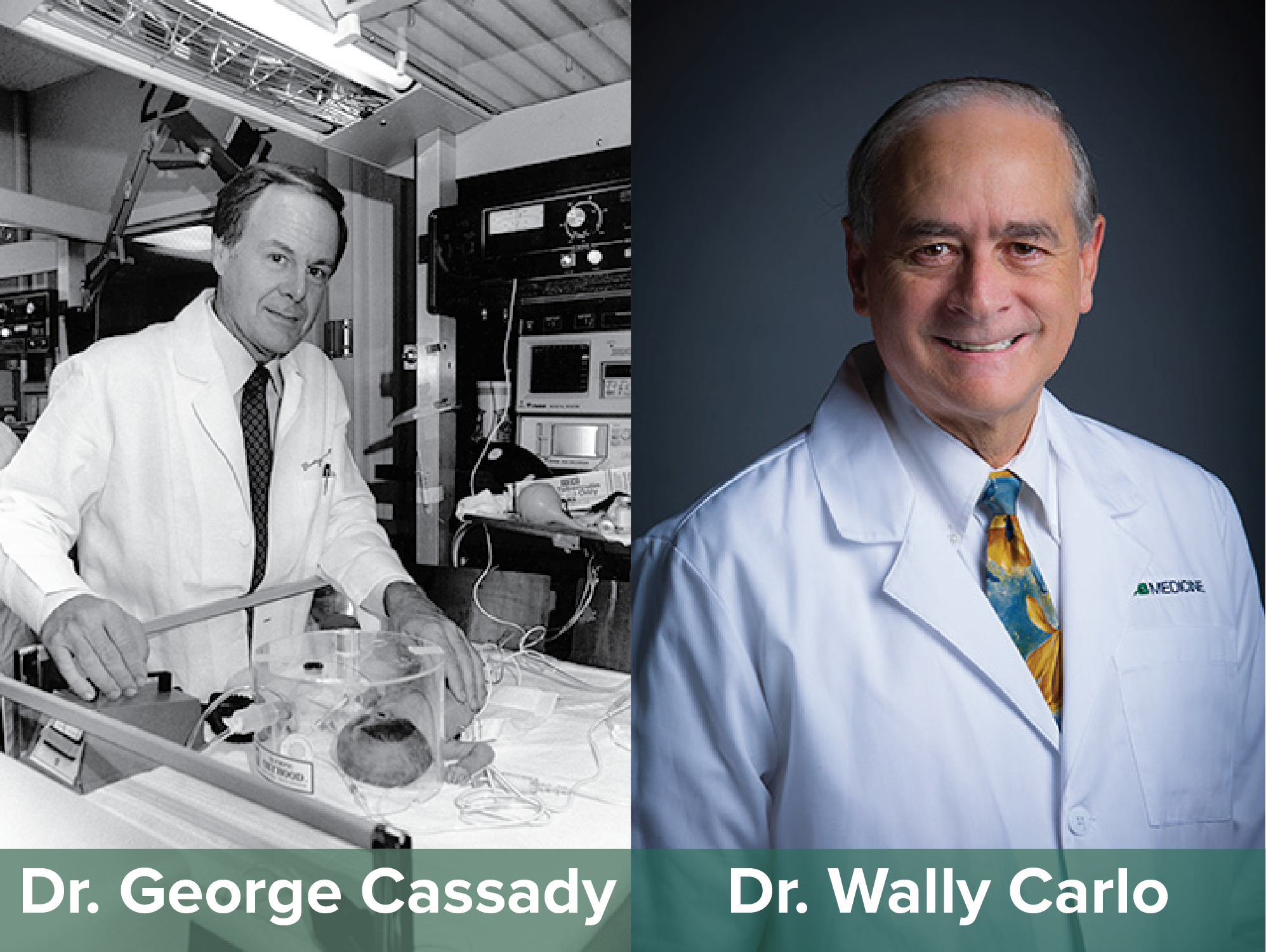
The Division of Neonatology was born with the arrival of Dr. George Cassady in July of 1964 as the chief of perinatology and director of nurseries after completing training at Duke University, Harvard University and the NIH. His final year of training was in neonatal physiology at Harvard University under the direction of the legendary Clement Smith. In his own words upon his arrival, Dr. Cassady said, “There were four nurseries on the 5th floor of Hillman – two ‘white’ on one side and two ‘colored’ on the other side of the delivery rooms – ‘regular’ & ‘premature’ nurseries. My first task was to convert the ‘colored’ nurseries into a single ‘High Risk’ nursery which had about 1,110 admissions during its initial year of operation. The ‘white’ nurseries became the ‘Well Baby Nursery’. The total deliveries was about 3,500 that year. Many threats to me and my family from the KKK for the ‘integration’!!”
During those early years, Dr. Cassady had a number of trainees, there was no official neonatal-perinatal fellowship then, and junior faculty but no official and funded faculty associates until 1980. Several of his early associates went on to significant leadership positions at other institutions in the US and abroad.
Dr. Joseph Philips joined the faculty as an assistant professor in 1980 after his fellowship in neonatal-perinatal medicine at the University of Florida where he studied in the laboratory of Sidney Cassin, Ph.D., a pioneer in the field of the pulmonary transitional circulation. Dr. Philips established the Perinatal Physiology Research Laboratory and continued work in the field of pulmonary transitional circulation and persistent pulmonary hypertension of the newborn. This laboratory continues today under the direction of Dr. Namasivayam Ambalavanan who arrived as a fellow in 1993 and remained on faculty upon completion of training and is now professor of Pediatrics with significant NIH and other agency funding.
Dr. Cassady and Dr. Philips were funded in the initial round of funding from National Institute of Child Health and Human Development (NICHD) for the Neonatal Research Network. The division’s participation in this important national, multi-centered consortium, which has produced numerous seminal studies, continues to the present day.
-
Dr. Carlo Becomes Division Director
Dr. Waldemar (Wally) Carlo arrived as director of the Division of Neonatology in 1991. He continued membership in the NICHD Neonatal Research Network and subsequently gained membership in the NIH-sponsored NICHD Global Network for Women’s and Children’s Health Research. Dr. Carlo has published hundreds of scholarly works and has positively affected healthcare for infants worldwide. He has received numerous prestigious awards including the Douglas K. Richardson Award in Perinatal and Pediatric Healthcare from the Society for Pediatric Research and the Virginia Apgar Award from the American Academy of Pediatrics.
The original newborn nurseries were located on the 5th floor of the New Hillman Building. They underwent extensive remodeling in the late 1980 to encompass space on the 4th and 5th floors. However, as census increased, satellite step-down nurseries were established in the adjoining Jefferson Tower building. The first NICU opened at Children’s Hospital of Alabama in the late 1980s under the direction of Dr. Raymond Lyrene. After several years the Children’s nursery expanded into two separate units. In 1991, the division established a community group to provide neonatology services to local hospitals outside the UAB and Children’s systems. This group has grown to cover most NICUs in the city and surrounding area.
-
The Division Continues to Grow
The ever-increasing census of the UAB RNICU led to its relocation to the Women and Infant’s Center in 2010. This state-of-the-art, all private room NICU has a capacity of 125 infants. It is the largest all private room NICU in the country and is one of the largest of any kind. Two state-of-the-art 25 bed NICUs opened in the Benjamin Russel Hospital at Children’s of Alabama in 2012. Combined, these NICUs constitute the largest academic neonatology service in the nation.
An accredited fellowship in neonatal-perinatal medicine was established in the late 1980s. More than 75 neonatologists from all over the world have been trained since the late 1970s. Many of these have assumed positions at prestigious institutions including chairs of pediatrics and directors of neonatology, while others have pursued careers in private practice.
The faculty currently numbers 22. Many current faculty members are NIH funded or are working towards this goal. Others are focused on quality improvement or simulation.
The division has made many significant contributions to the understanding of neonatal pathophysiology and disease over the years. Dr. Cassady made seminal contributions to our understanding of fluid and electrolyte physiology of the fetus and neonate while at UAB. Dr. Philips made important contributions to our understanding of the physiology of the transitional pulmonary circulation and the elucidation of the mechanism whereby Group B Streptococcus causes pulmonary hypertension in the newborn. More recently, the division has become a powerhouse of investigation into the pathophysiology and management of bronchopulmonary dysplasia. Additional areas of study include the pulmonary microbiome, the neonatal brain and the role of mitochondria in neonatal disease.
-
Division Leadership
Division Directors
George Cassady-1964 to the late 80s
Photo credit: UAB ArchiveWally Carlo- 1991 to present
-
Prominent Faculty
-

George Cassady
Dr. George Cassady, a native of California, joined the faculty of the Department of Pediatrics in 1964 as head of the Division of Neonatology. Dr. Cassady graduated from Duke Medical School in 1958 and completed his residency training at the same institution in 1960. He then served for two years as a clinical associate and medical investigator in the genetics unit at the NIH. From 1962 to 1964 he was a senior resident in pediatrics and fellow in neonatal physiology with Dr. Clement Smith at Harvard University.
When Dr. Cassady joined the Department in 1964 the neonatology unit at University Hospital was located on the third and fourth floors of the New Hillman Building on the corner of 20th Street and 7th Avenue South. By 1980, the unit had grown to 21 beds for premature/sick neonates with an average daily census of 19, and 95 beds for healthy newborns with a daily census of 47.
Dr. Cassady was an excellent leader who was not afraid to ruffle feathers in order to get things done. He had superb clinical skills and was a great motivator and teacher. He did not settle for anything less than excellence and was demanding of himself and his co-workers. He valued research and aggressively pursued funding. The culmination of his efforts occurred when he secured funds from the National Institute of Child Health and Human Development (NICHD) for the research network of neonatal intensive care units. He was funded on the first cycle, one of only seven institutions. This grant has been renewed multiple times and is still active today. The division under his direction provided exemplary education and a continuous flow of quality research at both basic and clinical levels. The fellowship program established by Dr. Cassady soon after his arrival at UAB has produced excellent clinical and basic research individuals in the field of neonatology, populating both academic medicine and private practice.
Dr. Cassady, unhappy with the unacceptably high rate of neonatal and infant mortality in Alabama, worked tirelessly to address the problem by working with the State Medical Association, the Alabama Chapter of the American Academy of Pediatrics (AAP) and the State Department of Public Health. He appealed to leaders in the community and asked for ideas and the collaboration of physicians for the purpose of reducing the tragic and unnecessary toll of infant deaths in Alabama. Since his call for action was issued in the State Medical Association Journal in 1968, neonatal outcomes have improved substantially, but unfortunately Alabama still ranks at the bottom of infant and newborn mortality statistics.
During his time as division director, Dr. Cassady recruited several neonatologists. Among them, Drs. David Wirtschafter, Joseph B. Phillips, Elaine Barefield, and others. George Cassady retired in 1989 and returned to California where he became director of neonatology and chairman of the Department of Pediatrics at Children’s Hospital of San Francisco.
-

Wally Carlo
In 1991, the department was successful in recruiting Dr. Wally Carlo from Rainbow Children’s Hospital in Cleveland to lead the Division of Neonatology. The arrival of Dr. Carlo was one of the most significant additions to the faculty because of his strong leadership skills and “can do attitude.” He immediately set up an open-door policy for all neonates from any referring hospital. He committed himself to the highest standards of care, strong research and collaboration with institutions across the USA and abroad. Dr. Carlo successfully secured a multi-institutional NIH grant for the Neonatal Network, plus many other grants, to support his and his collaborators research. He has become an internationally renowned neonatologist for his landmark studies in Zambia, India and Latin America. Dr. Carlo also created a system whereby a group of neonatologists in his division care for all neonates born at six other community hospitals, allowing for high standard of care and judicious use of resources. This model is still operative today and transformed the Neonatology Division into one of the top such units in the country in terms of productivity per faculty, size of research portfolio, international recognition and overall reputation.
-
Other prominent faculty
Numerous faculty members have come and gone over the years. A significant number have assumed leadership roles in prominent academic institutions upon leaving UAB. An incomplete listing includes Drs:
-George Cassady who went on to lead several divisions of neonatology and to hold other important leadership positions before his retirement.
-David Wirtschafter who took a prominent leadership position with Kaiser-Permanente,
-Clinton Joiner who moved first to Cincinnati and is now the Aflac Children’s Endowed Chair for Hematology, Director, Section of Hematology and Vice Chair for Research in the Department of Pediatrics at Emory University
-Siddhartha Tan who is division chief of Neonatal and Perinatal Medicine at the Detroit Medical Center’s Children’s Hospital of Michigan and Hutzel Women’s Hospital
-Robert Schelonka who is chief of Neonatology at Oreqon Health Sciences University
-Lance Prince who is now chief of Neonatology at UC San Diego
-Akhil Maheshwari, Josephine S. Sutland Professor of Newborn Medicine, Director, Eudowood Division of Neonatology and Vice-Chair (Integration), Department of Pediatrics, Johns Hopkins University.
-
Division of Pediatric Rehabilitation Medicine
-
Beginnings of the Division
In 2002, the UAB Department of Physical Medicine and Rehabilitation Medicine faced financial difficulties and the long term stability of the faculty dedicated to pediatric care was in jeopardy. The Department of Pediatrics negotiated the transfer of Dr. Charlie Law, the only remaining pediatric rehabilitation medicine faculty member, and started the UAB Division of Pediatric Rehabilitation Medicine. In 2004, Dr. Drew Davis became the division’s first fellow and upon completion of his training, he joined the faculty in 2005. Subsequently an ACGME accredited fellowship in pediatric rehabilitation medicine was established and trained Christian Niedzwecki, D.O., from 2009-2010. In 2011, Dr. Law resigned from the faculty and Dr. Davis assumed the position of division director.
-
Growth of the Division
In 2013, Dr. Paola Mendoza-Sengco joined the division upon completion of her fellowship training in pediatric rehabilitation medicine at Cincinnati Children’s Hospital Medical Center. Dr. Erin Swanson-Kimani joined the division in 2015 after completing a combined residency in general pediatrics and physical medicine and rehabilitation at Cincinnati Children’s Hospital Medical Center.
Since its inception, the division has provided a full continuum of services including inpatient consults, acute inpatient rehabilitation and multidisciplinary outpatient clinics. As the division has grown, two inpatient consult services have been developed to serve general inpatient rehabilitation consults and neonatal intensive care unit consults. The inpatient rehabilitation service admits approximately 100 patients for intensive inpatient rehabilitation annually. Outpatient services have expanded to three clinic locations at Children’s of Alabama Benjamin Russell Hospital for Children Main Campus, Children’s South and Children’s at Lakeshore. Outpatient clinical services at these locations include the General Rehabilitation Clinic, Muscular Dystrophy Association Clinic, Spina Bifida Clinic, Brachial Plexus Clinic, Neuro-Oncology Clinic, Home Ventilator Clinic, Hospital Follow-up Clinic, Spasticity Clinic, Movement Disorder Clinic, Concussion and Post-Concussion Concussion Clinic, NICU Follow-up Clinic, Pre-natal Spina Bifida Clinic, CRS Teen Transition Clinic, CRS Cerebral Palsy Clinic Metabolic Bone Clinic and GI/Rehabilitation Clinic.
The division serves as the primary training site for UAB physical medicine and rehabilitation residents’ pediatric rehabilitation medicine clinical rotations and routinely trains fellows from other divisions as well as pediatrics residents. UAB medical students rotate during their PM&R and pediatric rotations and electives and special topics courses are offered to UAB and visiting US and international medical students throughout the year. The division also provides all pediatric didactics for the UAB Physical Medicine and Rehabilitation Medicine lecture series.
Cynthia Wozow, D.O., joined the division in July 2020. She completed her residency at the William Carey College of Osteopathic Medicine in Hattiesburg, MS. She completed her residency in Physical Medicine & Rehabilitation at the University of Texas in San Antonio and her fellowship in Pediatric Physical Medicine & Rehabilitation at Baylor College of Medicine and Texas Children's Hospital.
-
New Research Expansion
In 2017 the division began a concerted effort to expand research efforts by creating secondary division appointments for research staff from around the UAB. The first was James Rimmer, Ph.D., Lakeshore Foundation Endowed Chair in Health Promotion and Rehabilitation Sciences, and director of the UAB/Lakeshore Research Collaborative. Subsequently, Harshvardhan Singh, PT, Ph.D., UAB School of Health Professions, and Laura Dreer, Ph.D. director, Psychological & Neuropsychology Clinical Research Services with the UAB Department of Ophthalmology and Visual Sciences, have received appointments with the goal of optimizing opportunities for generating new knowledge to positively impact the lives of children with disabling congenital and acquired health conditions. With support from Lakeshore Foundation and the UAB/Lakeshore Research Collaborative, the division established the Lakeshore Foundation Pediatric Rehabilitation Ph.D. Postdoctoral Research Position in 2018 with the goal of developing a pediatric focused rehabilitation and exercise research program.
Division of Pediatric Rheumatology
-
Early Pediatric Rheumatology Care in Alabama
As the department continued to grow, one of the most glaring deficiencies in was the lack of a stable pediatric rheumatology program. Dr. Joe Butler, who trained in pediatric rheumatology at the NIH, led the service for a brief period before his resignation in 1988. In 2000, Dr. Polly Ferguson, a board-certified pediatric rheumatologist was recruited from the University of Virginia. Unfortunately, she resigned her appointment to return to Iowa to help elderly parents. After her resignation, there were no board-certified pediatric rheumatologists in the entire state of Alabama for years. The national shortage of such specialists was particularly critical in the South.
The rheumatology clinic was staffed primarily by adult rheumatologists from the UAB program. In the early days, the clinic was staffed Dr. Howard Holley and later by Dr. Gene Ball. Dr. Holley said, “The children have a special place in my thoughts because I know what they’re going through. They’ve suffered more in their short lives than most people ever will. And you hardly ever find one that complains.” Dr. Louis Heck was the director of the program from 1980 until 2000. Upon his departure, Dr. Prescott Atkinson, a member of the Division of Immunology, assumed the responsibility for pediatric rheumatology before and after Dr. Ferguson’s tenure. Dr. Richard Jones, an adult rheumatologist in Tuscaloosa, also helped with clinics in Birmingham and Mobile.
-
Division is Established
The need for pediatric rheumatology specialists had to be quickly addressed. A plan was developed by partnering with the Arthritis Foundation of Alabama who committed to raise $1 million, and Children’s Hospital of Alabama, who committed $500,000 if it would be matched by UAB and agreed to the construction of a state-of-the-art clinic and an infusion therapy unit. Soon a $2 million endowment was established and a major recruiting effort was mounted. Dr. Randy Cron and his colleague, Dr. Tim Beukelman were recruited from the Children’s Hospital of Philadelphia. Dr. Cron was a nationally renowned pediatric rheumatologist with a successful research background, excellent clinical training and a proven mentor. For these reasons, he was able to recruit Dr. Beukelman as his junior partner. Mr. Ted Kennedy, a very successful Birmingham businessman, played a key role in the recruitment of Dr. Cron and later contributed funds to establish an endowed fellowship program for the division.
The many families with children with rheumatologic conditions and the faculty were delighted with the news. On September 10, 2007, the new Division of Pediatric Rheumatology Clinic at Children’s Hospital opened its doors in a brand-new facility.
-
Continued Growth of the Division
The Division of Pediatric Rheumatology has become very successful and continues to expand. The faculty has grown to five members plus one to three fellows per three years of training. The division provides state-of-the-art clinical care to all patients in Alabama and neighboring states. A satellite clinic operates in Mobile with every other monthly visits by a faculty member. There are also every other monthly clinics in Huntsville and Montgomery. In addition to the more typical rheumatologic conditions, the group has developed research programs and clinical expertise in such areas as macrophage activation syndrome, temporomandibular joint arthritis, juvenile spondyloarthropathy and several programs assessing safety and efficacy of therapeutic interventions. The national visibility of the faculty is outstanding, and the faculty record of invited lectures and scientific publications is equally remarkable. Current faculty members include Drs. Randy Cron, Melissa Mannion, Mathew Stoll, John Bridges and Emily Smitherman.