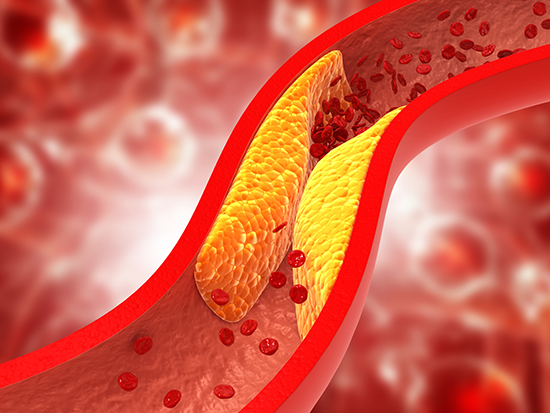
 These immune CD8 T cells may provide a target for treating the buildup of fatty lesions in the arteries called atherosclerosis.Aging is known to be a risk factor for the biological changes that create the dangerous buildup of plaque in arteries called atherosclerosis. Aging also induces a buildup of memory CD8 T cells, a type of immune cell, in mice and humans.
These immune CD8 T cells may provide a target for treating the buildup of fatty lesions in the arteries called atherosclerosis.Aging is known to be a risk factor for the biological changes that create the dangerous buildup of plaque in arteries called atherosclerosis. Aging also induces a buildup of memory CD8 T cells, a type of immune cell, in mice and humans.
While this buildup of plaque leads to the heart attacks and strokes that cause nearly one-third of deaths worldwide, the role of aging on CD8 T cells during atherosclerosis has been unclear.
Now a study in the journal Nature Aging, led by researchers at the University of Alabama at Birmingham and the University of Michigan, has shown that CD8 T cells are necessary and sufficient to enhance atherosclerosis in aging. This identifies these memory CD8 T cells as potential therapeutic targets of atherosclerosis in aging.
“There have been important advances in the development of T cell therapies for treating cancer, and our study paves the way for potential therapeutics targeting T cells to treat and prevent atherosclerosis in older adults,” said Daniel Tyrrell, Ph.D., corresponding author and assistant professor in the UAB Department of Pathology Division of Molecular and Cellular Pathology.
Unlike other mouse models for atherosclerosis, where mice have elevated blood lipid levels throughout their lives, Tyrrell and colleagues initiated atherosclerosis by giving mice an enzyme that degrades a receptor for low-density lipoprotein particles, or LDL, which in turn reduces cell uptake of fat from the blood. This was followed by 10 weeks of a high-fat Western diet that raised blood lipid levels and caused atherosclerosis. This 10-week period could be initiated in young mice or initiated when mice were old, after they had lived all their lives with normal blood lipid levels.
The researchers showed a key role for aging-mouse CD8 T cells in atherosclerosis in two ways. First, they used an antibody to deplete CD8 T cells in old or young mice before they initiated the disease process by knocking out the LDL receptor and starting the 10-week high-fat diet. They found that this depletion of CD8 T cells reduced atherosclerosis in aged mice, but not in young mice.
Second, they transferred spleen CD8 T cells from healthy aged mice or healthy young mice into recipient mice that lacked CD8 T cells, and then initiated disease by knocking out the LDL receptor and giving the high-fat diet. The researchers found that transfer of CD8 T cells from aged donors significantly enhanced three measures of atherosclerosis in the aorta threefold, compared to transfer of CD8 T cells from a young donor.
 Daniel Tyrrell, Ph.D.Much of the rest of the study created a comprehensive atlas of how T cells change with age in disease-free spleens and atherosclerotic plaques in mice. Single-cell RNA sequencing was used to reveal changes in gene expression and CD8 T cell types.
Daniel Tyrrell, Ph.D.Much of the rest of the study created a comprehensive atlas of how T cells change with age in disease-free spleens and atherosclerotic plaques in mice. Single-cell RNA sequencing was used to reveal changes in gene expression and CD8 T cell types.
They found that CD8 T cells that accumulate in atherosclerotic plaques in aging mice are primarily memory T cells, both effector memory T cells and central memory T cells, with few naive T cells represented. The memory T cells had cytotoxicity gene expression. Also, the CD8 T cells from aged and young aortas were more differentiated compared to CD8 T cells from young spleens. A large number of the effector memory T cells in aged plaque expressed the gene for granzyme K, an enzyme that is cytotoxic against target cells.
These mouse data were similar to a previous single cell RNA-sequencing study in older adults that showed most T cells within human atherosclerotic plaques were memory subtypes and were more cytotoxic and inflammatory in symptomatic patients versus patients without symptoms.
Other highlights of the study included: 1) finding increased CD8 T cell clonal expansion — as measured by T cell receptor sequencing — with aging and within atherosclerotic plaque, 2) finding that aging alters CD8 cell transcription in atherosclerosis, 3) finding that aging upregulates chemokine receptors in atherosclerosis, and 4) finding that about one-third of atherosclerotic T cells are gamma-delta T cells, whose role in atherogenesis is not fully understood.
The finding that most CD8 T cells in atherosclerotic plaques of aging mice are memory T cells, not naïve T cells, is similar to previous findings for atherosclerotic plaques from humans averaging 70 years of age. Tyrrell and colleagues re-analyzed that human T cell dataset and found that most CD8 T cells in the human atherosclerotic plaques also expressed granzyme K, with higher levels in symptomatic patients. “Thus, we found that aged murine atherosclerotic plaque CD8 T cells exhibit similarities to human atherosclerotic patients, which suggests that our findings in mice are similar to humans,” Tyrrell said.
The findings of this study support the original premise for this research, Tyrrell says — that the majority of chronic diseases, including atherosclerosis, are diseases of aged individuals.
Co-authors with Tyrrell in the study, “Clonally expanded memory CD8+ T cells accumulate in atherosclerotic plaques and are pro-atherogenic in aged mice,” are Kathleen M. Wragg, Judy Chen , Hui Wang, Jianrui Song, Muriel G. Blin, Abhinav Janappareddi, Sherri C. Wood and Daniel R. Goldstein, University of Michigan Department of Internal Medicine; and Chase Bolding, Donald Vardaman III, Kara Giles, Harrison Tidwell and Md Akkas Ali, UAB Department of Pathology.
Support came from National Institutes of Health grants AG068309, HL5569, AG028082, AI38347 and HL58003; and American Heart Association grant AHA89820.
At UAB, Pathology is a department in the Marnix E. Heersink School of Medicine.
