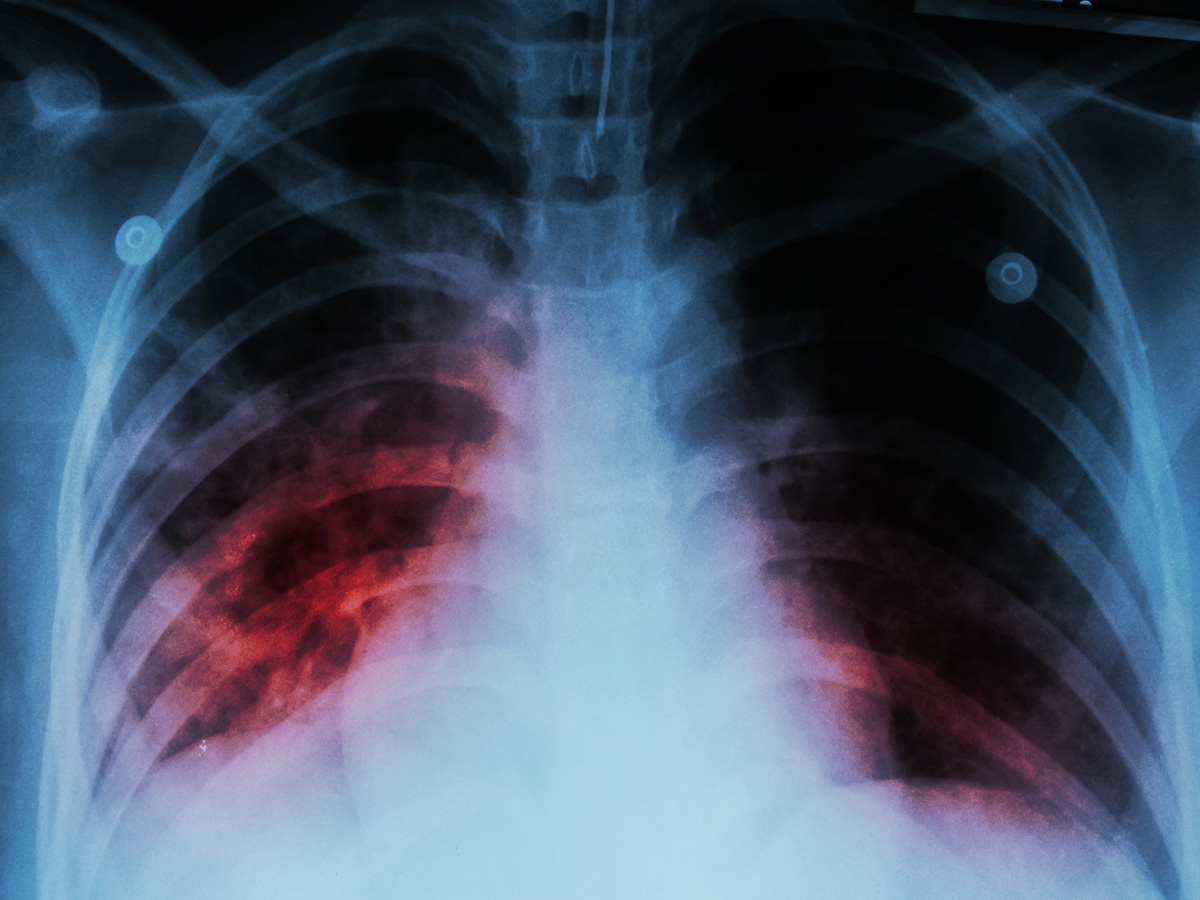
 Virginia Meikle, Ph.D. and Michael Niederweis, Ph.D. Tuberculosis is the world’s leading infectious cause of death, killing more than one million people each year.
Virginia Meikle, Ph.D. and Michael Niederweis, Ph.D. Tuberculosis is the world’s leading infectious cause of death, killing more than one million people each year.
When the antibiotic bedaquiline was introduced in 2012, it was the first new tuberculosis drug in over 40 years. Bedaquiline quickly became the key drug in all standard drug-resistant tuberculosis regimens globally. Unfortunately, clinical Mycobacterium tuberculosis strains rapidly become resistant to bedaquiline, predominantly by overexpression of MmpL5.
The proteins MmpL5 and MmpL4 are efflux transporters, critical pumps that help the pathogen M. tuberculosis grow by scavenging essential iron from the iron-deprived lung granulomas of its human host. The pumps secrete mycobactin molecules that then tightly bind external iron. The microbial pathogen then uses other molecular machinery to carry the mycobactins and their iron cargoes back into the cell. Unfortunately, overexpressed MmpL5 can also pump out bedaquiline as an unintended hitchhiker, making the bacteria drug-resistant.
Finding a way to disable the efflux transporters of M. tuberculosis with an inhibitor would strike a double blow — restore microbial sensitivity to antibiotic bedaquiline and break the cycle that gathers scarce iron. M. tuberculosis is poisoned and loses virulence when mycobactin efflux pumps cannot function.
Researchers at the University of Alabama in Birmingham and the University of Zurich, Zurich, Switzerland, have now solved the structure of MmpL4, a close homolog of MmpL5 that has the same function, they report in the journal Nature Communications.
“This study was the result of a fantastic collaboration with the group of Markus A. Seeger, Ph.D., University of Zurich, and provides the basis for a better molecular understanding of iron acquisition and drug efflux by M. tuberculosis,” said Michael Niederweis, Ph.D., UAB professor of microbiology. “The development of inhibitors targeting this secretion system could transform the treatment of drug-resistant tuberculosis.”
Virginia Meikle, Ph.D., a senior scientist in the UAB Department of Microbiology, did all the functional assays of this study and is a co-first author.
In some of the details of the study, the structure of purified MmpL4 protein was determined by cryogenic-electron microscopy. The first low-resolution structure, aided by docking with AlphaFold2, the artificial intelligence protein structure prediction system, showed the domain that spans the inner membrane of M. tuberculosis and much of the periplasmic domains (the periplasm is the space between the inner and outer membranes of many bacteria). However, no electron density was seen for an unusual 130 Å-long coiled-coil domain predicted by AlphaFold2. When that was replaced by a short linker, the researchers were able to determine a 3.0 Å cryo-electron microscopy structure of the truncated MmpL4.
 Besides their normal role, pump overexpression confers drug resistance. Knowing the structure is a step to disabling the pumps with inhibitors.The structure showed 12 transmembrane helices in two pseudo-symmetric bundles and two periplasmic subdomains.
Besides their normal role, pump overexpression confers drug resistance. Knowing the structure is a step to disabling the pumps with inhibitors.The structure showed 12 transmembrane helices in two pseudo-symmetric bundles and two periplasmic subdomains.
Experiments showed that the coiled-coil domain, whose predicted model extends from one of the periplasmic subdomains toward the outer membrane like a long antenna, was essential in both MmpL4 and MmpL5 for export of the siderophore mycobactin and for resistance to bedaquiline.
“We identified the predicted coiled-coil domain as crucial for mycobactin and bedaquiline export,” Niederweis said. “To our knowledge, it is the first coiled-coil domain described as an essential part of a membrane transporter.”
Another cryo-electron microscope structure of MmpL4 bound to desferrated mycobactin identified the precise binding site for mycobactin on the cytosol-exposed region of MmpL4, just inside the inner membrane. Single amino acid variant mutations identified which MmpL4 amino acid moieties at the binding site are essential, intermediate or non-essential for binding of mycobactin. Further work showed that MmpL4 binds bedaquiline at the same site as mycobactin.
Proton translocation is the energy that drives the efflux pumps, and single amino acid variant mutations of the presumed proton-coupling residues in MmpL4 and MmpL5 identified which ones are essential for proton translocation.
The researchers also serendipitously found that a mycobacterial biosynthesis cofactor, MbtL, forms a complex with MmpL4, indicating that mycobactin synthesis and export are coupled.
“The structural and functional insights presented in this study provide a basis for the rational design of drugs that simultaneously block mycobactin secretion and bedaquiline efflux by MmpL4 and MmpL5,” Niederweis said. “This will enable the development of urgently needed novel tuberculosis drugs that exploit synergistic effects of mycobactin poisoning and increasing the susceptibility of M. tuberculosis to bedaquiline.”
Co-authors with Niederweis, Seeger and Meikle of the study, “Structural basis of siderophore export and drug efflux by Mycobacterium tuberculosis,” are Jennifer C. Earp and Alisa A. Garaeva, University of Zurich.
At UAB, Microbiology is a department in the Marnix E. Heersink School of Medicine.