By: Austin Oslock, Med-Peds PGY4
“Thank you for taking the time to come see me,” the patient says with tears streaming down his face. You can see the gratitude in his eyes and hear it in his voice. Such appreciation felt for a simple doctor’s visit. The 35-year-old man sitting across from me weighs over 300 pounds and is wheelchair dependent. He hasn’t left his house in more than 6 months, except by ambulance.
His home has a wheelchair lift installed by a local non-profit, but the lift is broken and he has no other way to leave his home. Today’s visit is an intake visit for UAB House Calls, a home-based primary care program operated through the University of Alabama Birmingham. This is his first primary care visit in years. We sit in his bedroom, a cramped space, filled with boxes of medical supplies. A few years ago the patient was in a car accident and suffered multiple leg fractures. After the accident, he never regained his ability to walk, essentially losing his functional independence. He has young children, and he aspires to walk and play with his kids again. We work together to develop a plan forward.
In every House Calls visit, we ask our patients “what matters most.” For some patients, their goal is to regain function and independence; to get healthier, and to be able to leave their homes for reasons other than a doctor’s appointment. These patients hopefully go on to get stronger, and eventually “graduate” from the House Calls program. For others, their goal is to stay at home; to be comfortable and well cared for, surrounded by the people they love. They hope to avoid trips to the ER or hospitalizations. For each patient, we strive to help them achieve their goals through access to a robust primary care program in the comfort of their own home.
UAB House Calls was started in 2015 by one MD and an APP working out of the Geriatrics Clinic. It has now grown to 5 providers, 3 social workers, and a whole team of nurses, medical assistants, and case managers to deliver care to a panel of 300+ patients. The program aims to serve home-bound patients in the Birmingham area, up to 30 miles from the UAB hospital.
UAB House Calls cares for patients from all backgrounds -- with all kinds of medical conditions and social determinants. The program accepts both Medicaid and Medicare and doesn’t consider insurance type when screening patients. A day of house call visits may consist of driving from an elegant mansion, to a low-income housing apartment, to a senior living facility, to a farmhouse with livestock, to a singlewide trailer with a rat or roach problem. To be an effective house calls provider, one must acknowledge a patient’s living environment (and the challenges it may present), while also looking beyond these to deliver excellent, equitable, and unbiased care. Just as “a picture is worth a thousand words,” a visit to a patient’s home can tell you more about them and their health than a year’s worth of clinic visits.
When I complete my Internal Medicine residency training in June, I will be joining UAB House Calls to deliver care to patients in need. When asked why I am joining UAB House Calls, I tell people, “I’ve never felt more like a doctor than when I’m taking care of a patient in their home.” In addition, by visiting patients’ homes, I am able to easily appreciate the social determinants of health impacting their care. I can determine food insecurity by opening an empty fridge, health literacy by the arrangement of their daily medications, and transportation barriers by the number of stairs leading up to their apartment.
To qualify for UAB House Calls, a patient must be home-bound for any reason. In general, their condition must limit their ability to seek care at a typical primary care office. Our patients often fall into one of three categories: 1) disabled, 2) frail / elderly, or 3) medically complex (often resulting in frequent ER visits or hospitalizations). What does a UAB House Calls patient look like? They are a 20-year-old young man with Duchenne’s muscular dystrophy dependent on a tracheostomy & ventilator, a 95-year-old woman requiring 24-hour supervision due to severe dementia, a 53-year-old man with profound critical-illness neuropathy and chronic respiratory failure due to COVID pneumonia, and a 29-year-old man with a spinal cord injury resulting in multiple chronic wound infections and frequent hospitalizations.
The program provides care to many patients with chronic wounds. For those patients who have only Medicaid insurance, UAB House Calls serves a particularly important role. Did you know that Medicaid doesn’t cover home health nursing services for wound-care? Furthermore, the only wound-care products covered by Medicaid are tape, gauze, and normal saline. Any specialized wound-care products (Vashe wash, Mepilex, Medihoney etc.) must be purchased out-of-pocket at high cost to the family. For patients with severe wounds, UAB House Call nurses conduct visits to assist with wound cleaning and dressing changes. In addition to these visits, UAB House Calls delivers many of the typical services expected of primary care including medication management and vaccinations. We are also able to obtain imaging studies at home including x-rays, ultrasounds, ECGs, and echocardiograms.
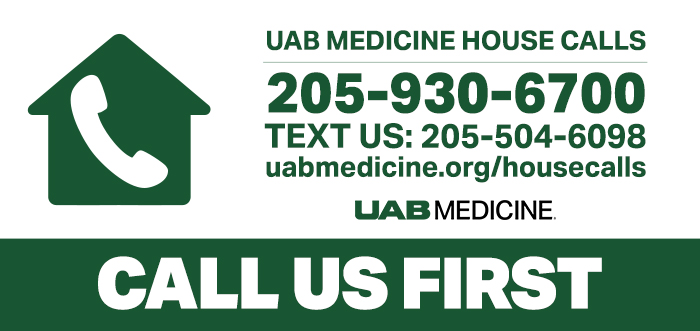
The goal of UAB House Calls is to deliver patient and family-centered comprehensive primary care. By doing this, we provide patients more quality days at home and reduce unnecessary hospitalizations. Our request to patients is simple, “When you are thinking about going to the hospital, call us first.” It’s even printed on the program’s refrigerator magnets! If a patient has a cough and fever, we can obtain an urgent chest x-ray (at home) and send in antibiotics for pneumonia all without a visit to the hospital. UAB’s program has been shown to reduce ED visits and hospitalizations by 40%. In addition, many of our patients are severely ill and approaching end-of-life. For these patients, UAB House Calls has helped 60-70% of our patients die at home instead of in the hospital. To accomplish this, we have early and frequent conversations about a patient’s values, passions, and goals of care. We ask what matters most. We help our patients to complete health care directives and portable DNAR forms. We encourage families to have these serious conversations outside of times of crisis, in the comfort and safety of their home.
As part of the UAB Tinsley Harrison Internal Medicine Residency Program, every resident rotates through a house calls program. Currently, residents are either paired with UAB House Calls or with the longstanding Veteran Affairs (VA) Home-Based Primary Care program (VA HBPC). Recently, UAB House Calls launched a 3rd year medical student elective embedded in their IM clerkship. In this elective, medical students spend one week shadowing providers, nurses, and social workers performing house call visits. At the end of each 3rd year’s week-long rotation, they write a reflection about their experience with home-based care. In these reflections, students often cite their time with House Calls as a transformative experience. They are struck by the team-work required in house calls, by the “whole person” care delivered, and by the mission to consider and to address social determinants in our patients. I am grateful to be joining a team that delivers such transformative care, while giving residents and medical students a unique glimpse into our patients’ lives. House Calls may seem like a novel concept, but instead it is a revival of historic medicine that will be an integral part in the future of health care.